Generic Drugs: What They Are, How They Save Money, and What You Need to Know
When you hear generic drugs, lower-cost versions of brand-name medications that contain the same active ingredients, meet the same safety standards, and work the same way in your body. Also known as generic medication, they are the backbone of affordable healthcare in the U.S. and around the world. You might think they’re weaker or less reliable, but that’s not true. The FDA requires them to be bioequivalent to the brand-name version—meaning they deliver the same dose, work the same way, and have the same risks and benefits. The only differences? The shape, color, or inactive ingredients—and the price, which is often 80% lower.
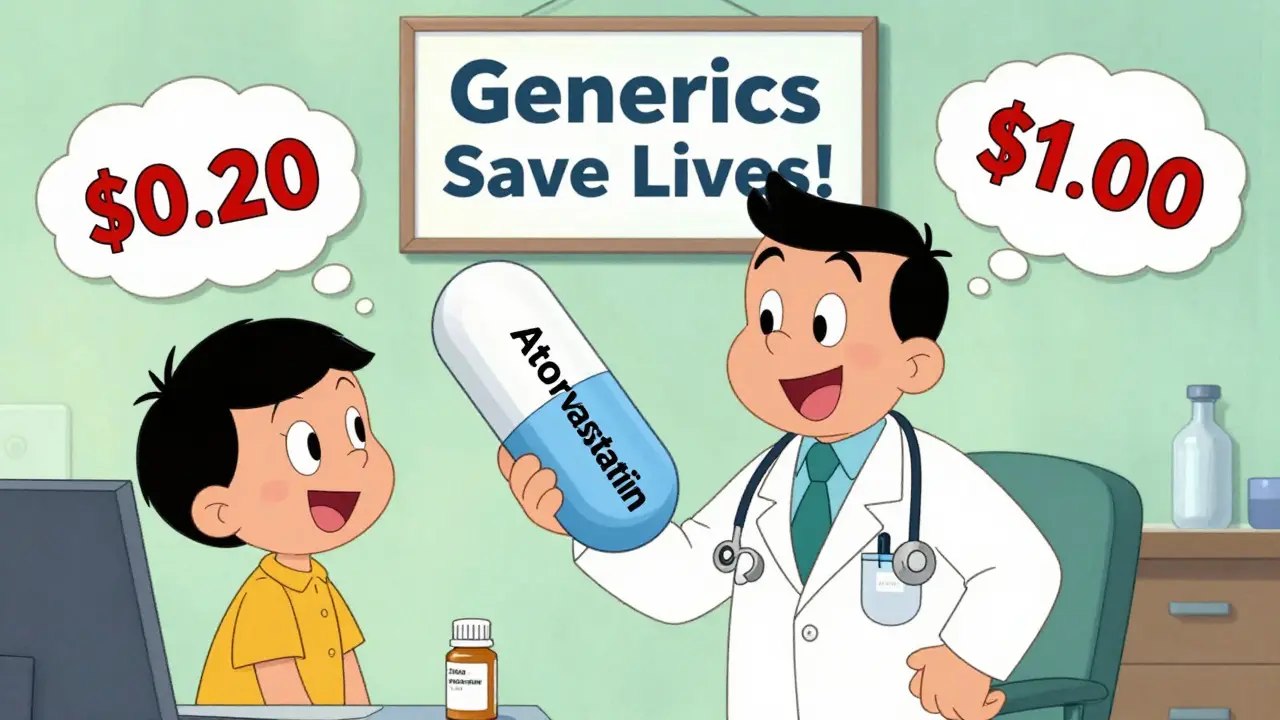
So why are they so much cheaper? It’s not because they’re made in shady labs. It’s because once a brand-name drug’s patent expires, other companies can make the same medicine without paying for the original research. This creates competition. Companies fight for your business by lowering prices. The drug pricing, the system that determines how much a medication costs based on market competition, regulatory approvals, and insurance rules doesn’t rely on price caps—it lets the market do the work. The FDA approves these generics fast, and the FTC steps in if companies try to block competition. That’s why you can buy generic lisinopril for $4 a month or metformin for less than $10 a refill.
But even cheap drugs can be hard to afford if you’re on a tight budget. That’s where generic copay assistance, programs that help patients pay for low-cost prescriptions through pharmacy discounts, nonprofit aid, or government support comes in. Medicare Extra Help, pharmacy coupons, and patient assistance programs from drugmakers can slash your out-of-pocket costs even further. You don’t need to be poor to qualify—many programs help people earning up to 400% of the federal poverty level. And if your insurance changes its formulary and drops your generic, you’re not stuck. You can appeal, ask for an exception, or switch to another approved version.
Some people worry about switching from brand to generic, especially with meds like thyroid drugs or seizure drugs. That’s fair. Small differences in inactive ingredients can affect how fast a drug is absorbed. But most people switch without any issue. If you notice changes in how you feel after switching, talk to your doctor—not your pharmacist, not your friend, not Google. Your doctor can check your blood levels or adjust your dose. You’re not alone: millions of Americans rely on generics every day, from statins for cholesterol to antibiotics for infections.
What you’ll find below isn’t just a list of articles. It’s a practical toolkit. You’ll learn how governments keep generic prices low, how to find financial help for medications you can’t afford, and how to avoid dangerous interactions—even with cheap drugs. You’ll see how people manage formulary changes, what to do when your insurance denies coverage, and how to read a prescription label so you never take the wrong dose. These aren’t theoretical guides. They’re written by people who’ve been there: struggling with bills, confused by labels, scared of side effects. They’re here to help you take control.