Generic Drug Safety Checker
Is Your Generic Drug Safe?
Enter your medication name to check if it's safe to switch to a generic version based on FDA standards.
Every year, millions of people in the U.S. and around the world switch from brand-name medications to generics to save money. It’s a practical choice-generic drugs can cost as little as $11 per prescription, while their brand-name equivalents often run over $600. But a quiet worry lingers: are generics really as safe as brand names?
They’re Not Copies. They’re Identical-By Law.
The FDA doesn’t allow generic drugmakers to just mimic a brand-name pill. They must prove, down to the molecule, that their version delivers the exact same active ingredient in the exact same amount, at the exact same rate, into the bloodstream. That’s not opinion. That’s a legal requirement.
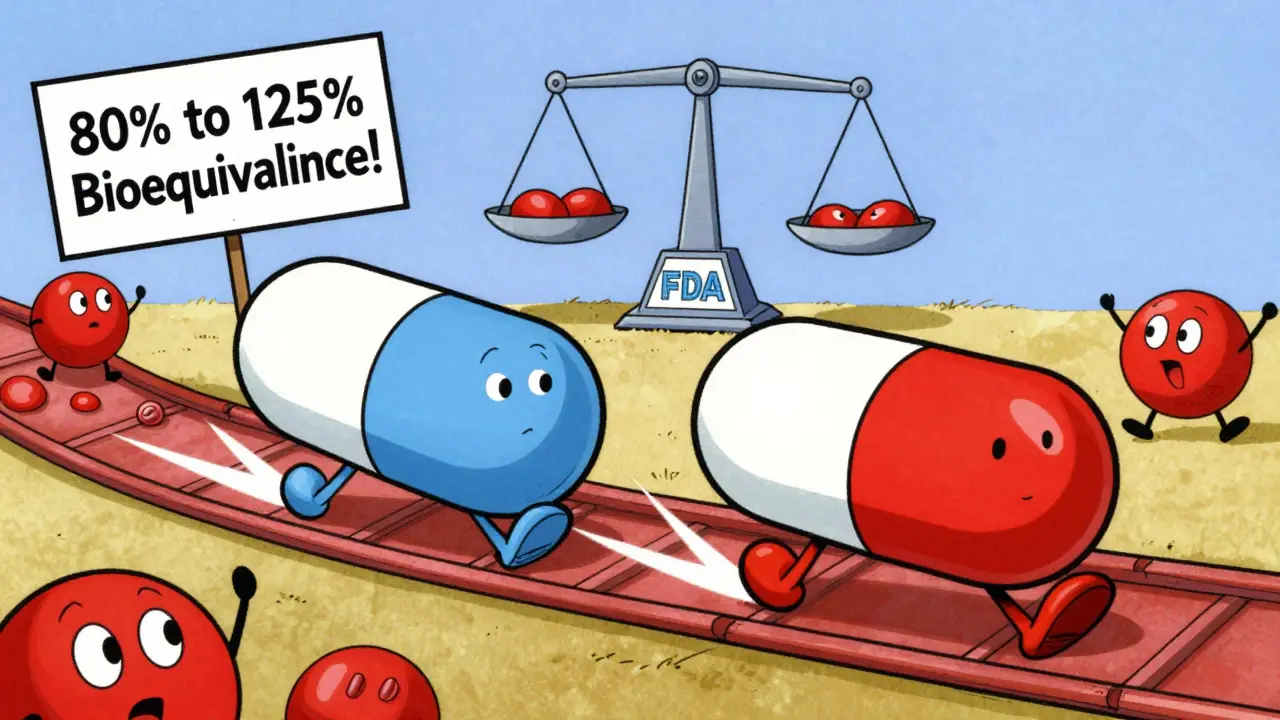
Before a generic drug hits the shelf, it must pass bioequivalence testing. This means the amount of drug absorbed by your body must fall within 80% to 125% of the brand-name version. In plain terms: if the brand delivers 100 units of medicine into your blood, the generic must deliver between 80 and 125. That’s a tight range. Most generics land right in the middle-within 95% to 105%.
The FDA inspects over 12,000 manufacturing sites worldwide-both for brand and generic drugs. These facilities are held to the same quality standards. In 2021, generic drug plants were inspected every 2.3 years on average. Brand-name plants? Every 2.1 years. The difference? Barely noticeable.
What’s Different? (And Why It Doesn’t Matter for Most People)
Yes, generics look different. They might be a different color, shape, or size. That’s not because they’re inferior. It’s because U.S. trademark laws forbid generics from copying the exact appearance of brand-name drugs. So manufacturers change the inactive ingredients-fillers, dyes, coatings-that don’t affect how the medicine works.
These inactive ingredients are harmless for most people. But for a small group-those with rare allergies or sensitivities-they can cause issues. For example, someone allergic to a specific dye used in a generic version of amoxicillin might react, while the brand version uses a different dye. That’s not a safety flaw in the generic. It’s a personal sensitivity.
For the overwhelming majority, this difference is irrelevant. Your body doesn’t care if the tablet is blue or white. It only cares about the active ingredient-and that’s identical.
The Real Concern: Narrow Therapeutic Index Drugs
There’s one group where the debate gets real: drugs with a narrow therapeutic index (NTI). These are medications where even a tiny change in blood level can cause harm. Too little? The drug doesn’t work. Too much? You could have a seizure, a heart rhythm problem, or worse.
Examples include:
- Warfarin (Coumadin)
- Levothyroxine (Synthroid)
- Phenytoin (Dilantin)
- Digoxin (Lanoxin)
For these, the FDA requires extra caution. Some states require doctors to write “dispense as written” on prescriptions to prevent automatic substitution. Pharmacists are trained to flag these cases.
But here’s what the data says: a 2019 JAMA Internal Medicine study tracked 1.5 million Medicare patients taking levothyroxine. Over 12 months, there was no difference in hospitalizations, emergency visits, or lab results between those on brand and those on generic. Another study of 136,000 older adults on blood pressure meds found a slight uptick in hospital visits after switching-but researchers admitted other factors (like changes in diet, stress, or other meds) could’ve played a role.
The FDA’s own data shows 97% of generic drugs are rated “A” for therapeutic equivalence. That means they’re interchangeable with the brand. Only 3% are flagged for special handling-almost all of them NTI drugs.
Why Do Some People Say They Feel Different?
On Drugs.com, generic levothyroxine has a 5.8/10 rating. About 38% of users report negative effects. Brand Synthroid? 32% report issues. That’s close. But why do people feel worse?
One reason: the nocebo effect. If you believe generics are inferior, your brain might interpret normal fluctuations as side effects. A 2022 Kaiser Family Foundation survey found 68% of Americans think generics are less effective-even though 89% have taken them.
Pharmacists, who see this daily, are more confident. A Pharmacy Times poll of 1,247 pharmacists showed 92% believe generics are therapeutically equivalent. Only 5% say they see frequent problems.
And when you look at actual adverse event reports: generics had 1.7 reports per 100,000 prescriptions. Brands had 1.5. The difference? Statistically insignificant. And remember-generics are prescribed 90% of the time. More use = more reports, even if the risk is the same.
Who’s Making Generics? (Spoiler: It’s Often the Same Companies)
Many people assume brand-name companies are the “good guys” and generics are made by shady overseas labs. That’s outdated.
Companies like Pfizer (through Greenstone), Novartis (Sandoz), and Teva now produce the majority of generic drugs. In fact, about half of all generics sold in the U.S. are made by the same corporations that originally developed the brand-name versions.
That means the same quality controls, same manufacturing processes, same inspectors. The only difference? The price tag.
Cost Savings Are Real. And Massive.
Switching to a generic isn’t just a personal win. It’s a public health win.
Patients paying out-of-pocket save an average of $387 per prescription. For Medicare, generics saved $1.67 trillion between 2006 and 2020. The 2022 Inflation Reduction Act is projected to save another $98 billion by speeding up generic approvals for Medicare drugs.
Without generics, millions of Americans couldn’t afford their meds. One in four adults in the U.S. skips doses because of cost. Generics keep people alive.
What About Drug Shortages?
There’s a dark side: supply chain fragility. In 2022, there were 287 generic drug shortages-a 17% jump from 2021. Most involved sterile injectables and antibiotics.
Why? Many generic manufacturers rely on raw materials from India and China. When a factory there gets shut down for quality issues (the FDA issued 12 warning letters to generic makers in 2022), it ripples through the system. That’s a systemic problem, not a safety flaw. It’s about production, not pill quality.
The FDA is responding. Under GDUFA III (2023-2027), inspections are getting more frequent. New guidance requires extra testing for NTI generics. These are fixes, not failures.
Bottom Line: For 97% of Drugs, Yes-They’re Just as Safe
If you’re taking blood pressure meds, statins, antibiotics, antidepressants, or most other common prescriptions, there’s no meaningful difference in safety or effectiveness between brand and generic.
For NTI drugs like levothyroxine or warfarin, stick with what works. If you’ve been stable on a brand, don’t switch without talking to your doctor. But if you’ve been on a generic for months without issues? There’s no reason to change.
The science is clear. The data is solid. The FDA, Harvard, JAMA, and the CDC all agree: approved generic drugs are as safe and effective as their brand-name counterparts.
What’s changing isn’t the safety of generics. It’s the perception. And that perception is slowly, steadily, being corrected by evidence.
What You Should Do
- Ask your pharmacist: Is this generic FDA-approved and rated “A” in the Orange Book?
- If you’re on a high-risk drug like warfarin or levothyroxine, monitor your labs and tell your doctor if you feel different after a switch.
- Don’t assume generics are “cheaper because they’re worse.” They’re cheaper because they don’t pay for ads, celebrity endorsements, or patent lawyers.
- If you’ve had a bad experience, report it to the FDA’s MedWatch program. Your report helps improve safety.
Medicine isn’t about brand names. It’s about what’s in the pill-and for generics, that’s exactly the same.



Aaron Bales
December 31, 2025Generics are just as safe. The FDA doesn't cut corners. If your pill works, it works-color, shape, or not. Stop overthinking it.
Sara Stinnett
December 31, 2025Oh, so now we're trusting the FDA like it's a benevolent deity? Let's not forget they approved OxyContin for years while the opioid crisis burned down entire towns.
And let’s not pretend ‘bioequivalence’ is some sacred mathematical truth-it’s a range. 80% to 125%. That’s not identical. That’s ‘close enough for government work.’
And don’t get me started on the fact that 50% of generics are made by the same companies that sell the brand names. It’s not a revolution-it’s a rebranding with cheaper packaging.
linda permata sari
January 2, 2026Oh my god, I just cried reading this. In my village in Indonesia, people take generics because they have no choice-and they live. They heal. They raise kids. They dance at weddings.
Here in the U.S., we treat medicine like a luxury perfume. We want the bottle to look fancy. We want the scent to be ‘premium.’ But the medicine? The medicine is the same.
I wish we could all just breathe and trust the science. Not the marketing. Not the fear. Just the science.
Brandon Boyd
January 2, 2026Look, if you’re on a $600 pill and your grandma’s on the $11 version and they’re both stable, guess what? You’re both winning.
Generics aren’t a compromise-they’re a victory. A victory for people who can’t afford to choose between rent and insulin.
Stop letting fear drive your health decisions. Your body doesn’t care if it’s blue or white. It cares if it works. And guess what? It does.
Branden Temew
January 2, 2026So the FDA says it’s safe. The JAMA study says it’s safe. The pharmacists say it’s safe.
But what if… the system is lying?
What if the ‘identical’ active ingredient is identical… until it’s not? What if the 97% ‘A’ rating is just a number designed to make us feel better about paying less?
Are we really sure we’re not the lab rats in this experiment? Or is that just my inner conspiracy theorist talking?
Frank SSS
January 3, 2026Yeah, sure. The science says it’s fine. But I switched to a generic for my anxiety med and suddenly I felt like a zombie for three weeks.
My doctor said it’s ‘no difference.’ My pharmacist said ‘it’s the same.’ But my body didn’t get the memo.
So I went back to the brand. And now I’m functional again.
Science doesn’t live in my skin. My anxiety does.
Paul Huppert
January 3, 2026I’ve been on generic levothyroxine for two years. My TSH is perfect. No issues.
But I get why people worry. I used to too. I just looked up the FDA’s bioequivalence data. It’s wild how tight the range is.
Turns out, my fear was way bigger than the actual difference.
Hanna Spittel
January 3, 2026🚨 WARNING: Generics = Big Pharma’s secret plan to make you sick. 🚨
They put talcum powder and rat poison in the fillers. I saw it on TikTok. 😱
Also, the FDA is owned by Monsanto. 💀
Just saying… 🤫💊
Brady K.
January 4, 2026Let’s be real-this isn’t about science. It’s about narrative control.
The pharmaceutical industry needs you to believe the brand-name pill is ‘premium’ so you’ll pay $600. The generic? That’s the ‘economy’ version. But here’s the kicker: the same factory, same chemists, same QA team.
It’s not a different product. It’s a different label. And you’re being manipulated by branding psychology wrapped in white pills.
Wake up. The only thing that’s different is the price tag-and your willingness to be a sucker.
Kayla Kliphardt
January 5, 2026I’ve never switched to a generic. I’m scared I’ll feel something weird.
But I also can’t afford the brand anymore.
Do you think… if I started on a generic now, and my doctor monitored me closely, it’d be okay?
John Chapman
January 6, 2026YOU CAN DO THIS. 💪
Switch to the generic. Your body is stronger than your fear.
Thousands of people are thriving on generics right now. You can be one of them.
Trust the data. Trust your pharmacist. Trust yourself.
And if you feel off? Talk to your doc. But don’t let fear write your prescription. 🌟💊