
More than 28 million Americans will experience an eating disorder in their lifetime. That’s not a distant statistic-it’s someone you know. Maybe it’s the classmate who always skips lunch, the coworker who disappears after meals, or the teenager who won’t look in the mirror. These aren’t just about food. They’re about control, pain, and survival. And left untreated, they kill.
What Anorexia and Bulimia Really Look Like
Anorexia nervosa isn’t just being thin. It’s a brain disorder where fear of weight gain overrides hunger, logic, and even the will to live. People with anorexia often have a body weight far below what’s healthy for their height and age. But here’s the truth most people miss: less than 6% of those with eating disorders are classified as "underweight" by medical standards. You can’t tell someone has anorexia just by looking at them. Bulimia nervosa is different in appearance but just as dangerous. It’s a cycle of binge eating-consuming large amounts of food in a short time-followed by purging. Vomiting, laxatives, fasting, or excessive exercise are used to undo the binge. One in ten people with bulimia develops swollen cheeks from repeated vomiting, a sign many don’t recognize as part of the disorder. Unlike anorexia, people with bulimia often maintain a normal weight, making it easier to hide. Both disorders come with physical damage. Anorexia can cause heart failure, bone loss so severe it mimics old age, and organ shutdown. Bulimia erodes tooth enamel, ruptures the esophagus, and throws electrolytes out of balance-leading to sudden cardiac arrest. The body doesn’t care if the behavior is "mental" or "emotional." It responds with damage.The Hidden Death Toll
Anorexia has the highest death rate of any mental illness. One person dies every 52 minutes from an eating disorder. That’s over 10,200 deaths each year in the U.S. alone. For every death, dozens more struggle silently. Suicide accounts for nearly a third of these deaths. People with anorexia are 18 times more likely to attempt suicide than those without an eating disorder. Bulimia isn’t far behind, with a mortality rate nearly double that of the general population. The statistics are grim, but they don’t tell the whole story. Behind each number is someone who felt trapped. Someone who believed they were worthless unless they controlled their body. Someone who thought no one could help.Why Most People Never Get Help
Only 27% of women with eating disorders by age 40 or 50 ever receive treatment. For bulimia and binge eating disorder, fewer than half ever seek help. Why? One reason: stigma. Many believe eating disorders are a choice, a phase, or a cry for attention. They’re not. They’re complex brain disorders with genetic, biological, and environmental roots. Half the risk for binge eating disorder is inherited. Another reason: access. There are only about 35 specialized residential treatment centers in the entire U.S. with a total of 1,200 beds. That’s less than 0.004% of the 30 million people affected. Wait times are brutal. One person on Reddit waited 27 months for care after being diagnosed with severe anorexia and a BMI of 14.5. Insurance denials are rampant. In a 2022 survey, 68% of people with eating disorders reported at least one insurance denial. Some needed 3 or more denials before getting approval. One person raised $78,000 on GoFundMe to pay for 90 days of treatment. The system is broken.
What Actually Works: Evidence-Based Care
Not all treatment is equal. Many therapists still use outdated methods. But science has moved forward. There are now proven, evidence-based approaches that work. For adolescents with anorexia, Family-Based Treatment (FBT) is the gold standard. Parents take charge of meals and recovery-not therapists, not the patient. In 12 months, 40-50% of teens recover with FBT, compared to just 20-30% with traditional individual therapy. It’s simple, powerful, and backed by decades of research. For adults with bulimia or binge eating disorder, Enhanced Cognitive Behavioral Therapy (CBT-E) is the most effective. It doesn’t just target eating behaviors. It addresses the underlying thoughts: "I’m not good enough," "My worth is tied to my weight," "If I eat this, I’ll lose control." After 20 sessions, 60-70% of patients stop bingeing and purging. That’s not improvement-it’s remission. And now, for the first time ever, there’s a medication approved specifically for binge eating disorder: lisdexamfetamine (Vyvanse). In clinical trials, it led to a 50.9% remission rate-more than double the placebo group. It’s not a cure, but it’s a tool. A real, FDA-approved tool.What Treatment Actually Involves
Treatment isn’t just therapy. It’s medical, nutritional, and psychological. First, doctors check vital signs, heart rhythm, and electrolytes. Many patients arrive with dangerously low potassium or heart rates below 40. Refeeding syndrome-a dangerous shift in fluids and minerals-can happen when calories are increased too fast. It’s why medical supervision is non-negotiable. Nutritionists don’t just hand out meal plans. They help rebuild trust with food. For someone who hasn’t eaten in days, starting with 1,200 calories a day feels overwhelming. Progress is slow. Gaining a pound a week is a win. Therapy focuses on breaking the cycle. For bulimia, that means interrupting the binge-purge loop. For anorexia, it’s challenging the belief that being thin equals safety. Dialectical Behavior Therapy (DBT) helps with emotional regulation. Motivational interviewing helps people find their own reason to recover-because no one can be forced into healing.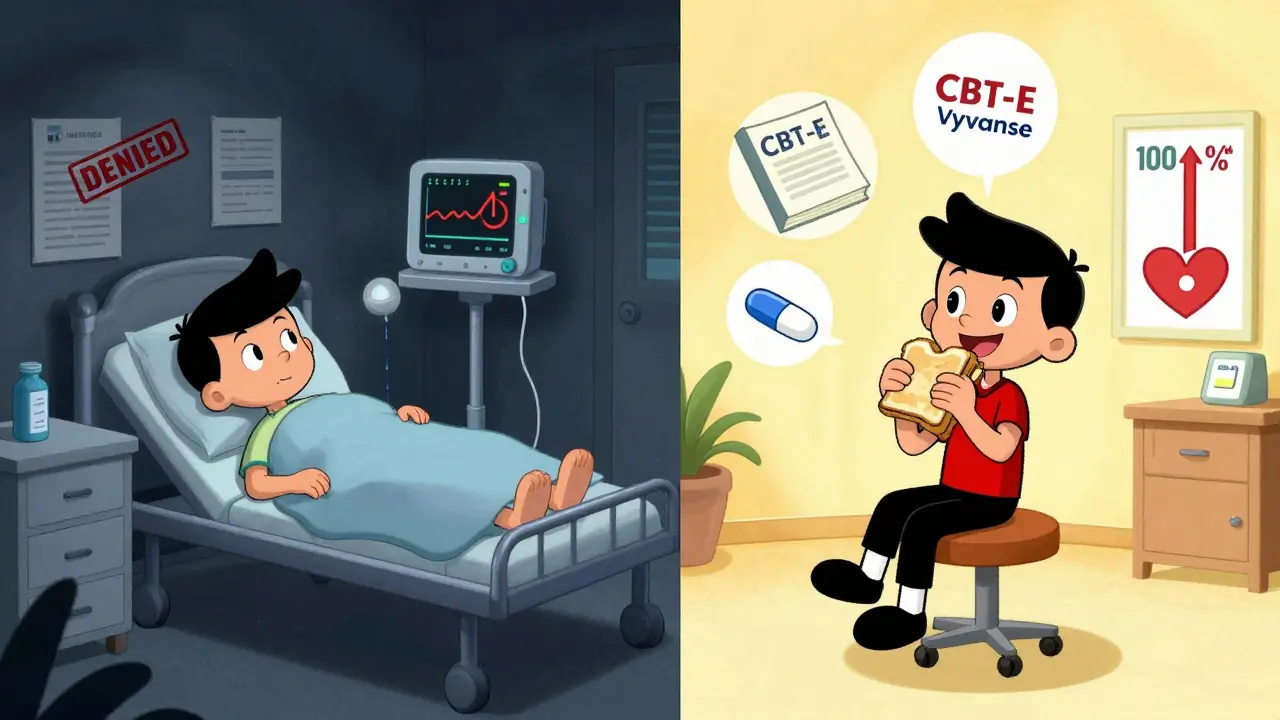
The System Is Failing, But Change Is Possible
The data shows we know how to treat these disorders. We just don’t do it. Only 12% of treatment centers use standardized tools like the Eating Disorder Examination Questionnaire (EDE-Q) to track progress. Only 43% follow evidence-based protocols. Rural areas are nearly invisible-22% of rural counties have zero specialists. Children under 12 are being hospitalized at rates up 119% since 2012. The system is collapsing under demand. But there are glimmers of hope. Telehealth is expanding access. Apps like Recovery Record have shown 32% greater symptom reduction than standard care. The 2023 Mental Health Parity Act led to $3.2 million in fines for insurers who denied care. The NIH is funding a $25 million study to find early biological markers in children. Recovery isn’t linear. Relapse is common. But it’s not failure-it’s part of the process. The key is early intervention. People who start treatment within three years of symptoms have a 65% chance of full remission. Wait longer, and the odds drop.What You Can Do
If you’re struggling: reach out. Even if you’re scared. Even if you think no one will understand. Call the National Eating Disorders Association helpline. Text "Help" to 741741. You are not alone. If you know someone who might be struggling: don’t wait for them to ask for help. Say something. "I’ve noticed you’ve been skipping meals. I care about you. Can we talk?" Don’t comment on weight. Don’t give advice. Just be present. If you’re a clinician: get trained. FBT and CBT-E require 120-180 hours of specialized instruction. Don’t wing it. Lives depend on it. If you’re an insurer or policymaker: enforce parity laws. Fund treatment centers. Cover what science says works. The cost of inaction is $64.7 billion a year-and thousands of lives.Recovery Is Possible
One woman, after seven years of bulimia, finally got CBT-E through a university clinic. Her binge-purge episodes dropped from 14 times a week to two. Another, after a 30-day residential program, gained 15 pounds and learned how to sit with discomfort without turning to food or restriction. Recovery doesn’t mean being perfect. It means being alive. It means having meals with friends without shame. It means looking in the mirror and not hating what you see. It means knowing your worth isn’t measured in pounds or calories. The path is hard. But it’s not impossible. And it’s worth it.Can you recover from anorexia or bulimia?
Yes. Recovery is possible, and many people fully recover. With evidence-based treatment like Family-Based Treatment for adolescents or Enhanced Cognitive Behavioral Therapy (CBT-E) for adults, 40-70% of patients achieve long-term remission. Recovery takes time, support, and often medical care, but it’s not rare. People go on to live full, healthy lives after treatment.
Are eating disorders only a problem for young women?
No. While eating disorders are more common in young women, they affect people of all genders, ages, and backgrounds. Men make up about 40% of cases, and diagnosis rates in boys and older adults are rising. The stereotype of a thin teenage girl is outdated and dangerous-it keeps men, older adults, and people of color from getting help.
Is weight the best indicator of an eating disorder?
No. Less than 6% of people with eating disorders are medically classified as underweight. Many with bulimia or binge eating disorder are of normal or higher weight. Eating disorders are about behavior, thoughts, and emotional distress-not body size. Judging by weight delays diagnosis and increases risk.
What’s the most effective treatment for bulimia?
Enhanced Cognitive Behavioral Therapy (CBT-E) is the most effective treatment for bulimia. Studies show 60-70% of patients stop bingeing and purging after 20 sessions. It targets the core thoughts driving the behavior, not just the symptoms. Medications like SSRIs help some, but CBT-E remains the gold standard.
Why do insurance companies deny eating disorder treatment?
Insurance companies often deny care because they classify eating disorders as "behavioral" or "non-medical," even though they cause life-threatening physical complications. Many plans limit the number of therapy sessions or require patients to be "medically unstable" before approving care. This delays treatment and increases long-term costs. Federal laws like the Mental Health Parity Act are meant to stop this-but enforcement is inconsistent.
Can medication cure an eating disorder?
No medication can cure an eating disorder alone. But lisdexamfetamine (Vyvanse) is the first FDA-approved drug for binge eating disorder, and it helps reduce binge episodes in about half of users. Medication works best when combined with therapy. For anorexia and bulimia, therapy and nutritional rehabilitation remain the foundation-medication is a supplement, not a solution.
How long does treatment usually take?
There’s no set timeline. Recovery can take months or years. For adolescents with anorexia, Family-Based Treatment typically lasts 12 months. Adults with bulimia often see major improvement in 20 sessions of CBT-E. But full recovery-meaning no relapse, healthy eating habits, and stable mental health-can take 2-5 years. Patience and persistence matter more than speed.
What’s the biggest barrier to getting help?
The biggest barrier is access. There aren’t enough treatment centers, specialists, or insurance coverage. Wait times for intensive programs can be over four months. Rural areas have almost no providers. Many people give up before they even start. Stigma and shame play a role, but the system’s failure to scale evidence-based care is the real obstacle.


steve rumsford
January 7, 2026This post hit me in the chest. I used to binge and purge for years and no one noticed because I was 'normal weight.' The shame was worse than the hunger.
LALITA KUDIYA
January 7, 2026In India we dont talk about this at all. My cousin starved herself for years and family said shes just being dramatic. No one knew how to help. This needs to change
Poppy Newman
January 8, 2026I love how you included CBT-E and FBT. So many therapists still treat this like a diet issue. 🙏
Anthony Capunong
January 9, 2026This is why America needs to stop letting foreigners run our healthcare. We have the best science in the world but some bureaucrat in D.C. says no to treatment because it's 'too expensive.' Pathetic.
Aparna karwande
January 10, 2026You think this is bad? In my village in Uttar Pradesh, girls who refuse to eat are called weak. They’re forced to marry at 14. At least here we have therapy. In India, we have silence and shame.
Ayodeji Williams
January 11, 2026LMAO so now its a brain disorder? My cousin did this for attention. She got 30k on gofundme and now shes on a cruise. Real struggle my ass
Kyle King
January 11, 2026They’re lying. Eating disorders are a hoax created by Big Pharma to sell Vyvanse. The FDA is in bed with the pharmaceutical industry. You think your BMI matters? The government wants you to believe you’re broken so they can control you.
Kamlesh Chauhan
January 11, 2026This is why I dont trust science anymore. One study says this one says that. My uncle starved himself for 2 years and then just ate a burger and it was fine. No therapy needed
Emma Addison Thomas
January 12, 2026I’m from London and I’ve seen the NHS struggle to keep up. We have brilliant clinicians but the waiting lists are brutal. It’s heartbreaking to watch someone deteriorate while they wait for a slot.
Anastasia Novak
January 13, 2026Let’s be real - the entire system is a performance art piece designed to make privileged people feel morally superior while the actual suffering is buried under layers of jargon and insurance denials. FBT? CBT-E? Vyvanse? Cute acronyms for a broken machine. The real issue isn’t treatment - it’s that we’ve turned human pain into a bureaucratic checklist. We don’t need more studies. We need people to stop looking away. You don’t need a PhD to say, ‘I see you’re hurting.’ But we’ve outsourced compassion to clinicians with 12-hour waitlists and EHRs that freeze every time you try to save a patient’s life. And don’t get me started on how insurance companies treat recovery like a luxury subscription service. You’re not a patient. You’re a risk factor. And if you’re not underweight enough? You’re not worth the paperwork. I’ve watched my sister die in slow motion while her insurance demanded she ‘prove’ she was dying. She was 19. She had a 13.8 BMI. They said she was ‘stable.’ Stable? She was counting heartbeats between sobs. And now? The system is still running. Still denying. Still pretending this is about calories when it’s about a world that told her she wasn’t enough - and then refused to help her prove otherwise.
Jonathan Larson
January 13, 2026The empirical evidence supporting Family-Based Treatment and CBT-E is unequivocal, and the systemic failures in access, reimbursement, and provider training represent not merely policy gaps but moral failures of the highest order. To permit preventable mortality to persist due to administrative inertia is to violate the foundational tenets of medical ethics: beneficence, nonmaleficence, and justice. We must advocate not merely for funding, but for structural reformation - for the normalization of early intervention, the dismantling of weight-based diagnostic bias, and the institutional prioritization of evidence over economics. Recovery is not a privilege; it is a right. And we, as a society, have abdicated our duty.