
Have you ever been handed a prescription for a brand-name drug and seen the price tag-$500, $1,000, even $2,000 a month-and wondered why there’s no cheaper version available? It’s not that generics don’t exist. They’re everywhere. But for some drugs, no matter how long the patent has been out, there’s still no generic option. And the reasons aren’t simple. They’re tangled in patents, chemistry, legal tricks, and corporate strategy.
Patents Aren’t the Whole Story
Most people think if a drug’s patent expires, generics automatically show up. That’s not true. A patent gives a company 20 years of exclusive rights from the day it’s filed. But that’s just the start. The clock doesn’t start ticking when the drug hits the market-it starts when it’s first filed, often years before the drug is even approved. By the time the FDA gives the green light, a drug might already have 7 or 8 years of patent life used up. That leaves only 12 to 13 years to make back the billions spent on research. To stretch that time, companies file secondary patents on everything from the pill’s coating to the way it’s taken. These aren’t new drugs. They’re tiny tweaks. But under U.S. law, each one can add more exclusivity. Take Nexium, for example. When the patent for Prilosec (omeprazole) expired in 2001, AstraZeneca had already patented esomeprazole-the mirror-image molecule-and rebranded it as Nexium. It worked. Patients switched. Sales soared. And generics for omeprazole didn’t touch Nexium until 2014.Complex Drugs Can’t Be Copied
Not all drugs are made the same. Some are simple chemicals you can replicate with a lab and a recipe. Others? Not so much. Take Premarin. It’s a hormone therapy made from the urine of pregnant horses. It contains a mix of 10 or more estrogen compounds-some known, many not fully understood. You can’t just synthesize it in a factory. You can’t isolate the exact mix. Even if you tried, the FDA requires generics to be bioequivalent, meaning they must behave the same way in the body. With Premarin, no one’s been able to prove a generic version matches the original. So, even though the patent expired decades ago, there’s still no generic. Biologics are even harder. These are drugs made from living cells-like Humira for arthritis or Enbrel for autoimmune diseases. They’re not chemicals. They’re complex proteins. Even small changes in how they’re grown or purified change how they work. That’s why generics for these drugs aren’t called generics at all-they’re called biosimilars. And they require 12 years of data exclusivity before they can even be considered. The first biosimilar for Humira didn’t reach U.S. shelves until 2023, seven years after the patent expired. Why? Because the manufacturer filed dozens of overlapping patents to block competitors.Manufacturing Is a Minefield
Even if the active ingredient is simple, the delivery system can be a nightmare. Think of an inhaler like Advair Diskus. The drug inside might be easy to copy, but the way it’s aerosolized, the pressure of the canister, the way the powder flows-all of that matters. Change the propellant or the valve design, and the dose you get could be too low-or too high. The FDA requires extra testing for these kinds of drugs, and it’s expensive. Many generic companies just walk away. Same goes for extended-release pills. Prozac Weekly, for example, slowly releases fluoxetine over seven days. Replicating that timing means getting the right mix of inactive ingredients-fillers, binders, coatings-that control how fast the drug dissolves. One tiny mistake, and the drug hits too fast or too slow. That’s dangerous for conditions like epilepsy or heart rhythm disorders, where even a 5% difference can cause seizures or arrhythmias. So the FDA demands more proof. And that means more time. More cost. Fewer companies willing to try.
Corporate Tactics That Delay Generics
There’s a dark side to this game. It’s called product hopping. A company sees its patent about to expire, so it tweaks the drug just enough to get a new patent-maybe changes the pill shape, adds a new coating, or switches from a daily pill to a once-a-week version. Then it stops selling the old version. Patients are forced to switch. Generics can’t be made for the old version because it’s no longer on the market. And the new version? Still under patent. The EpiPen is a textbook case. Mylan kept updating the design-new colors, new packaging, new needle shields-each time filing a new patent. Even though the active ingredient, epinephrine, had been around for decades, the device itself was patented. That kept generics out for over 20 years. When generics finally came, they were still more expensive than they should’ve been because the market had been artificially kept small. Then there’s pay-for-delay. Brand-name companies pay generic manufacturers to hold off on launching their version. The FTC found 297 of these deals between 1999 and 2012. One deal paid $1.2 billion to delay a generic version of the antidepressant Zoloft. These deals cost consumers an estimated $3.5 billion a year.Why Some Drugs Stay Expensive Forever
The numbers don’t lie. In 2022, 12% of prescriptions were for drugs with no generic alternative-but those drugs made up nearly 25% of total drug spending. The average price for a brand-name drug with no generic? 437% higher than its generic counterpart. For cancer drugs, nearly 70% have no generic option. Why? Because they’re complex, expensive to make, and the patient pool is small. Companies don’t want to risk millions on a drug that only 5,000 people take a year. Even when generics do appear, they don’t always work the same. Some patients report that generic versions of thyroid meds like Synthroid or seizure drugs like Lamictal feel different. That’s not just in their head. For drugs with a narrow therapeutic index-where the difference between a helpful dose and a toxic one is tiny-even a 5% variation in absorption can matter. The FDA allows generics to vary by up to 20% in how they’re absorbed. For most drugs, that’s fine. For others? It’s risky.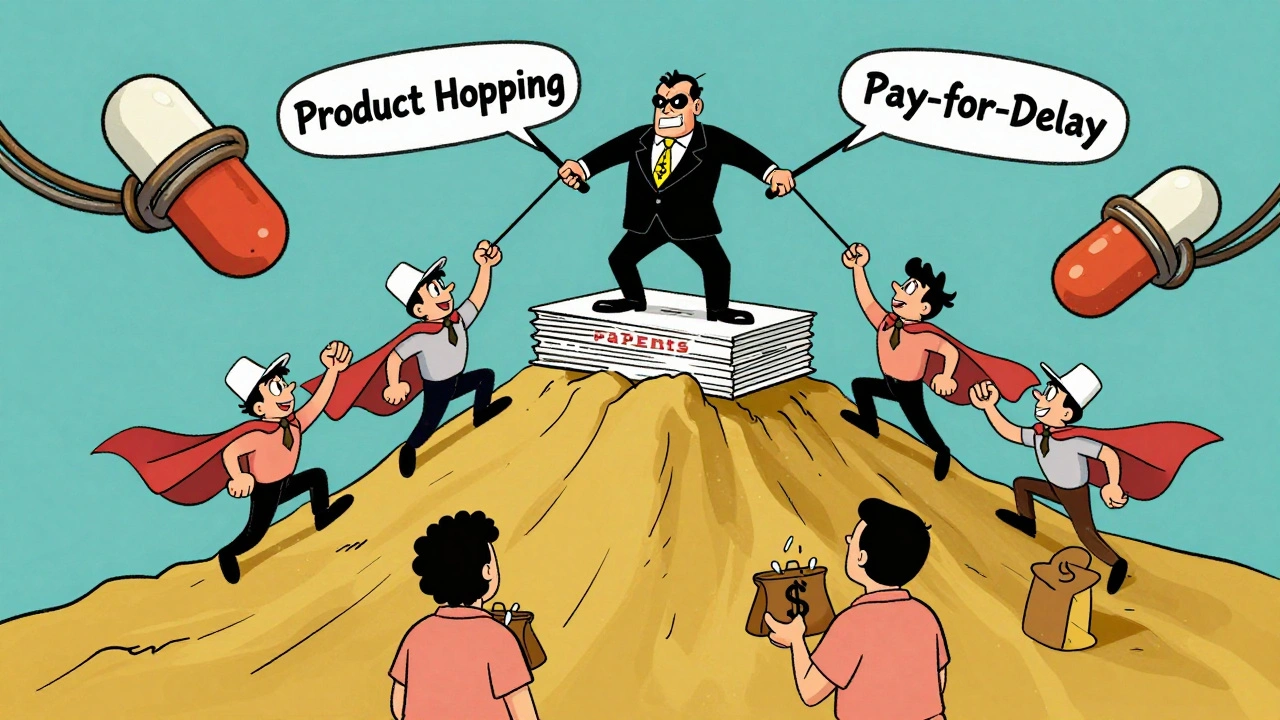
What’s Changing-and What’s Not
The FDA has started cracking down. The CREATES Act of 2019 forces brand-name companies to sell samples to generic makers so they can test their versions. Before that, many refused, claiming safety concerns. Now, they can’t. The 2022 Generic Drug User Fee Amendments (GDUFA III) sped up reviews for complex generics. In 2022 alone, the FDA approved 27% more complex generics than in 2021. Biosimilars are also on the rise. There were 32 approved in 2022. By 2025, that number could hit 75. But here’s the hard truth: Some drugs will never have generics. Insulin formulations. Rare disease treatments. Ultra-complex biologics. These aren’t just hard to copy-they’re nearly impossible. The science isn’t there yet. And even if it were, the cost to prove safety would be higher than the market is worth.What You Can Do
If you’re paying top dollar for a drug with no generic, talk to your doctor. Ask if there’s another drug in the same class that does the same job but has a generic version. For example, if you’re on Viibryd (vilazodone) for depression, sertraline might work just as well-and cost a fraction. Check the FDA’s Orange Book. It lists every patent and exclusivity period for every approved drug. You can see when a drug’s protections expire. Pharmacists can help you read it. And if you’re on Medicare Part D, ask about cost-sharing programs. Some plans offer better coverage for non-generic drugs if you appeal. You’d be surprised how often it works. The system isn’t broken. It’s working exactly as designed-for the companies that built it. But it’s not designed for you. And that’s why awareness matters. The more people understand how this works, the harder it becomes for these delays to fly under the radar.Why don’t all brand-name drugs have generic versions even after the patent expires?
Not all drugs can be easily copied. Some, like biologics or complex formulations, require advanced manufacturing and extensive testing to prove they work the same way. Others are protected by multiple overlapping patents that extend exclusivity beyond the original 20-year term. Companies also use legal tactics like product hopping or pay-for-delay deals to block generics from entering the market.
Are generic drugs as safe and effective as brand-name drugs?
For most drugs, yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent-meaning they’re absorbed in the body at the same rate and to the same extent. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or certain seizure meds-small differences in absorption can matter. Some patients report different experiences, and in those cases, sticking with the brand may be recommended.
What is a biosimilar, and how is it different from a generic?
A biosimilar is a version of a biologic drug-like Humira or Enbrel-that’s made from living cells. Unlike traditional generics, which are exact chemical copies, biosimilars are highly similar but not identical to the original. They require more testing and clinical trials to prove safety and effectiveness. They’re also subject to 12 years of data exclusivity before they can be approved, compared to just a few years for chemical generics.
Can I switch from a brand-name drug to a generic if my doctor hasn’t suggested it?
Yes, but talk to your doctor first. Pharmacists can substitute generics unless the prescription says "dispense as written" or "no substitution." For most medications, switching is safe and saves money. But for drugs with narrow therapeutic windows-like those for epilepsy, thyroid disorders, or blood thinners-it’s best to get your doctor’s approval. Some patients do better on the brand, and that’s okay.
How can I find out when a drug will have a generic version?
Check the FDA’s Orange Book, which lists all patents and exclusivity periods for approved drugs. You can search by brand name and see when exclusivity ends. Websites like GoodRx also track upcoming generic launches. But remember: even after exclusivity ends, it can take months or years for generics to appear due to legal battles or manufacturing delays.




Stephanie Bodde
December 5, 2025Ugh I just got hit with a $900 copay for my thyroid med last month 😭 Why does this even happen? I’m not rich, I just need to live. 🙏
Philip Kristy Wijaya
December 5, 2025Patents are a legal fiction designed to enrich shareholders not patients and you know it the entire pharmaceutical industry is a cartel masquerading as science the FDA is complicit and the so called biosimilars are just rebranded placebo with a fancy label
Jennifer Patrician
December 7, 2025They’re hiding the real reason. The government owns the patents through NIH research but lets pharma monopolize them. The same people who run the FDA used to work for Pfizer. You think that’s coincidence? Wake up. This isn’t capitalism. It’s corporate feudalism.
Mellissa Landrum
December 7, 2025lol so now its the feds fault? the real issue is we let big pharma bribe congress and now we pay for it with our lives. why do you think insulin cost 300 in usa and 10 in canada? because they dont let corporations rape the public here. its not rocket science its greed plain and simple
Mark Curry
December 8, 2025It’s strange how we accept this as normal. We build rockets to Mars but can’t make a pill affordable. Maybe the problem isn’t the science-it’s what we value. We reward profit over people. And we’re surprised when it breaks.
Jimmy Jude
December 8, 2025They’re not just delaying generics-they’re erasing the possibility of healing. Every time a drug stays expensive, someone dies waiting. This isn’t business. This is slow murder dressed in white coats and quarterly reports. I’m not angry. I’m devastated.
Mark Ziegenbein
December 10, 2025One must consider the epistemological underpinnings of pharmaceutical innovation wherein the commodification of molecular structures becomes a metaphysical exercise in capital accumulation masked as medical progress the biosimilar paradigm represents not innovation but mimicry without ontological equivalence and the FDAs regulatory framework is predicated upon a flawed utilitarian calculus that privileges market efficiency over biological fidelity
Rupa DasGupta
December 12, 2025India makes 40% of the world's generics but we can't export them to the US because of these stupid patent traps. You think this is about science? It's about control. They want you dependent. And they're winning.
an mo
December 12, 2025Let’s not confuse complexity with exploitation. The cost of bioequivalence testing for extended-release formulations is $20M+. The market for niche oncology drugs is 5k patients/year. ROI negative. This isn’t greed-it’s actuarial math. The system isn’t broken. It’s rational. You just hate the outcome.
aditya dixit
December 14, 2025My dad used to take a brand-name heart med that had no generic. We paid $700 a month. Then one day, a generic appeared. Same pill. Same results. Cost $12. He cried. Not from joy. From anger. We were robbed for years. And no one told us.
Lynette Myles
December 16, 2025Pay-for-delay is illegal but still happens. The FTC doesn’t enforce it. Why? Because the lobbyists write the rules. Simple.
Annie Grajewski
December 17, 2025so like... if you're on lamictal and switch to generic and suddenly feel like a zombie who forgot how to breathe... yeah that's not in the manual. but hey at least the stockholders got their dividend 💅
ashlie perry
December 18, 2025they’re not even trying anymore. just charge more. pretend it’s science. laugh while you bank. i’m not mad. i’m just done.
Juliet Morgan
December 19, 2025I know someone who got kicked off their brand-name epilepsy med because their insurance forced a generic. Had a seizure at work. Lost their job. Now they’re on disability. It’s not just money. It’s safety. And no one listens.