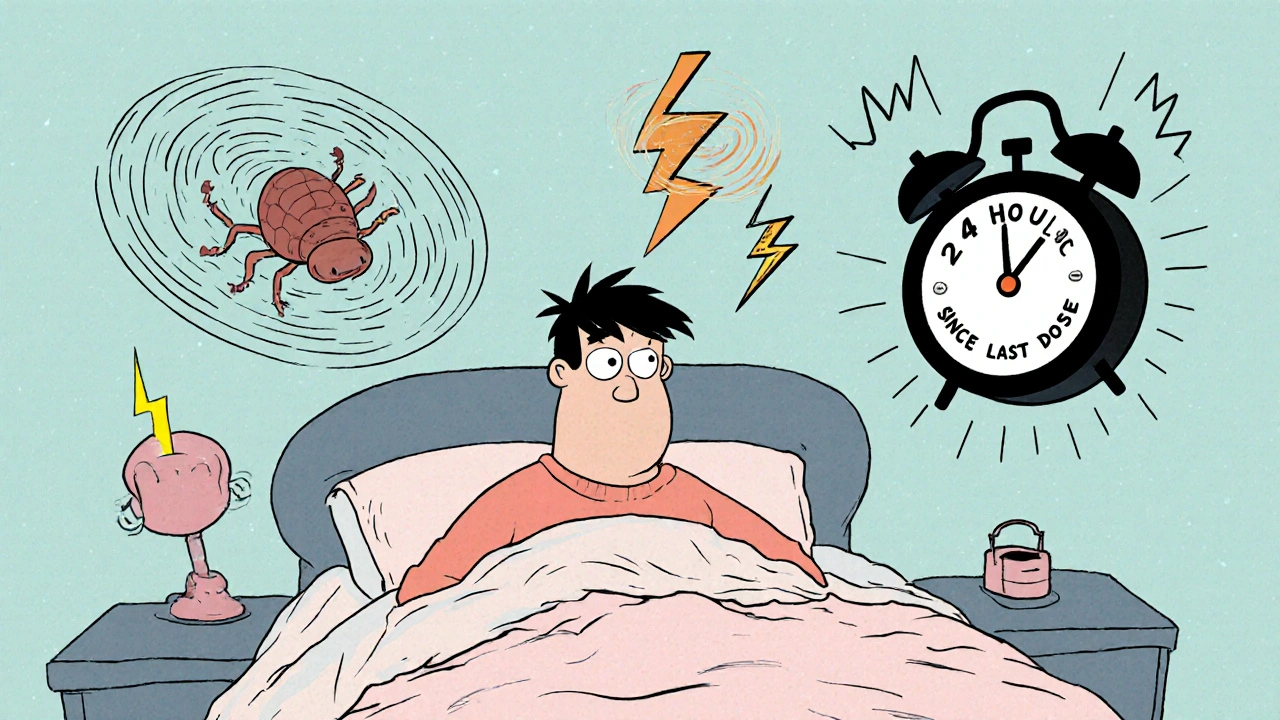
Brain Zaps: What They Are, Why They Happen, and How to Manage Them
When you stop or switch antidepressants, your brain doesn’t always adjust smoothly. One of the most unsettling side effects people report is brain zaps, sudden, brief electrical shock-like sensations in the head that can radiate to the neck or limbs. Also known as electroshock sensations, they’re not seizures or strokes—they’re a neurological response to changes in serotonin and other neurotransmitters. These aren’t rare. Studies tracking antidepressant discontinuation show up to 50% of people experience them, especially after stopping SSRIs or SNRIs cold turkey.
Brain zaps usually show up within days of reducing your dose or switching meds. They’re often tied to antidepressant withdrawal, a set of physical and emotional symptoms that occur when the brain loses its adapted chemical balance. But they’re not the only sign—many people also get dizziness, nausea, or intense dreams. What makes brain zaps so startling is how they feel: like a quick zap, flicker, or jolt inside your skull. Some say it’s like a camera flash going off behind their eyes. Others feel it in their ears or throat. They’re brief—usually under a second—but can happen dozens of times a day.
They’re not dangerous on their own, but they’re a clear signal your nervous system is out of sync. The good news? They usually fade within weeks if you stop tapering too fast. The key is slowing down. If you’re switching from one antidepressant to another, cross-tapering, gradually reducing the old drug while slowly adding the new one, cuts brain zaps by more than half. Skipping doses or switching too quickly? That’s when they spike. Even one missed pill can trigger them in sensitive people.
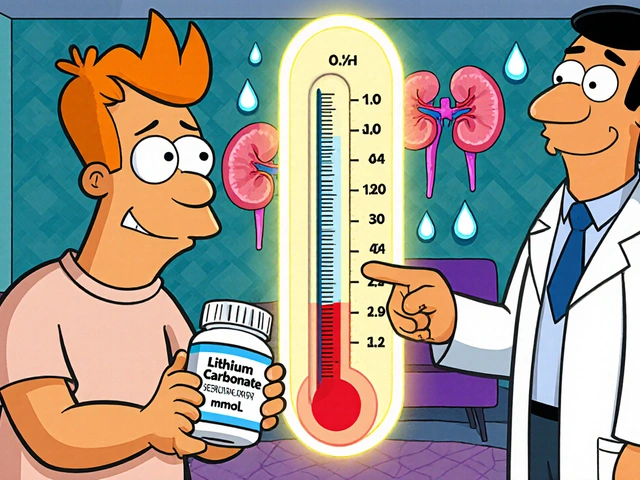
It’s not just about the drug you’re on—it’s about your brain’s history. People who’ve been on antidepressants for over a year, or who’ve had multiple switches before, are more likely to get them. So are those with a history of anxiety or migraines. And while no pill stops brain zaps outright, some doctors suggest adding a tiny dose of fluoxetine (Prozac) temporarily. It’s long-acting, so it smooths the transition. Others use magnesium or omega-3s, though evidence is limited. What works best? Patience and a slow, controlled plan.
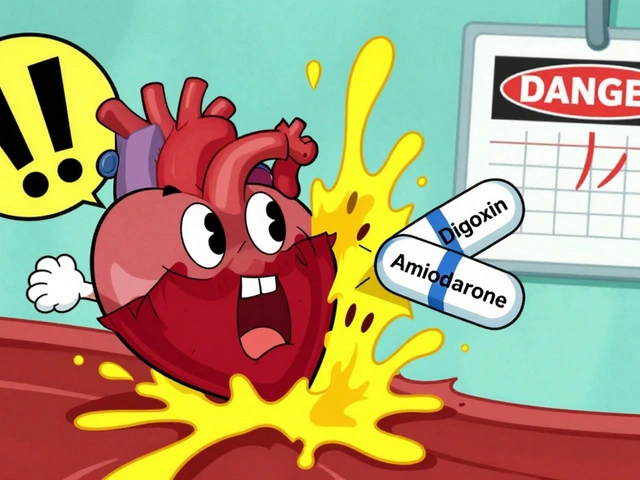
You’re not imagining this. These sensations are real, documented, and more common than most doctors admit. If you’re going through this, you’re not alone—and you don’t have to tough it out blindly. Below, you’ll find real guides from people who’ve navigated this exact issue. Some explain how to taper safely. Others break down why generics sometimes make it worse. A few show you how to spot when brain zaps are part of something bigger, like serotonin syndrome. Whether you’re thinking about stopping your meds, already switched, or just trying to understand what’s happening, the posts here give you the clear, no-fluff facts you need to take control.