Antidepressant Discontinuation Risk Calculator
Assess Your Discontinuation Risk
This tool estimates your risk of experiencing discontinuation syndrome based on your antidepressant and tapering approach.
Your Risk Assessment
Recommended Action:
Stopping antidepressants isn’t as simple as just skipping a pill. For many people, it triggers a cascade of physical and mental symptoms that can feel terrifying - like the depression is coming back, or worse, like something is seriously wrong with your body. These aren’t signs of addiction. They’re not weakness. They’re antidepressant discontinuation syndrome, a real, well-documented physical reaction to stopping or reducing these medications too quickly.
What Exactly Is Antidepressant Discontinuation Syndrome?
Antidepressant discontinuation syndrome happens when your body has adapted to the presence of the medication, and then you remove it. It’s not psychological dependence. You don’t crave the drug. You don’t get high off it. But your brain has changed how it handles serotonin, norepinephrine, or other neurotransmitters over weeks or months of use. When the drug leaves your system, your brain doesn’t instantly snap back to its old balance. That mismatch causes symptoms.
The term was originally pushed by drug companies to make antidepressants seem less like addictive substances - but doctors now agree: this is a true withdrawal syndrome, similar to what happens with benzodiazepines or even alcohol. The American Academy of Family Physicians confirmed its existence in 2006, and since then, research has only strengthened that view. It’s not rare. It’s not imaginary. It’s predictable - if you know what to look for.
The Symptoms: The FINISH Mnemonic and More
Doctors use the mnemonic FINISH to remember the most common signs:
- Flu-like symptoms: Fatigue, muscle aches, chills, headaches, nausea - reported in up to 78% of cases.
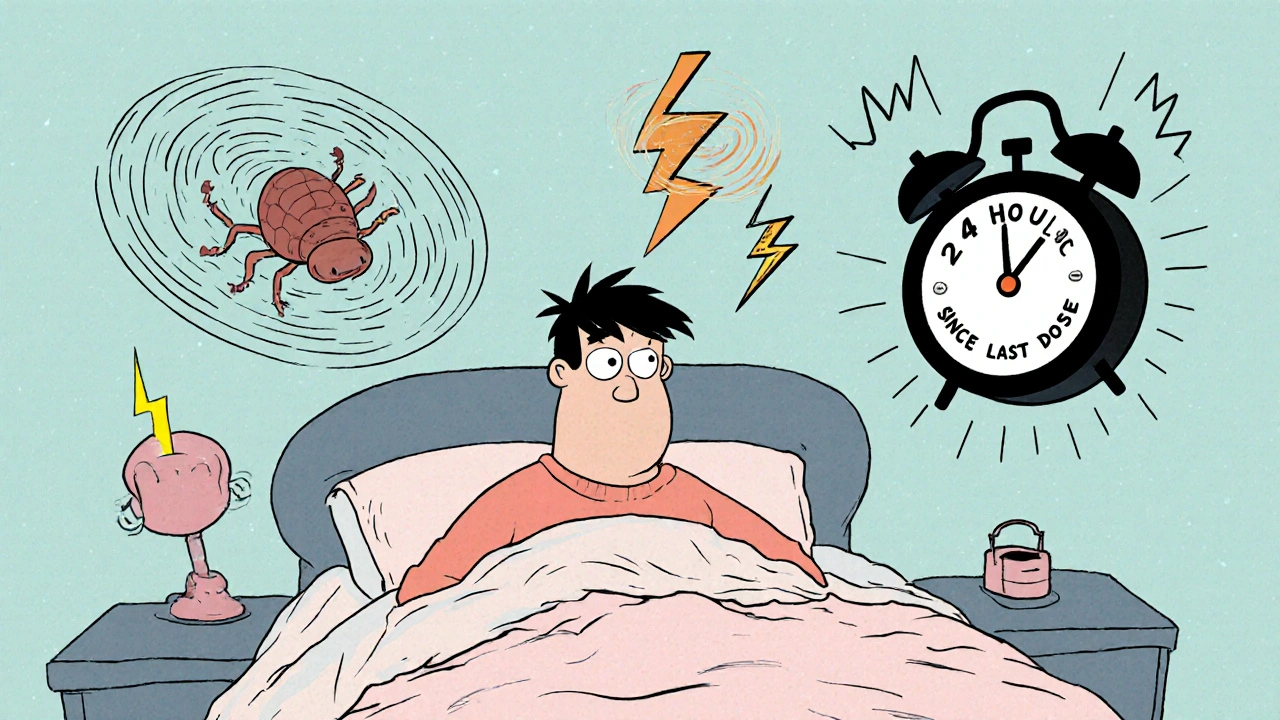
- Insomnia: Trouble falling asleep, waking up in the middle of the night, or having vivid, disturbing dreams.
- Nausea: Feeling sick to your stomach, sometimes vomiting.
- Imbalance: Dizziness, vertigo, unsteadiness when walking - like you’re on a boat.
- Sensory disturbances: Tingling, numbness, or the infamous ‘brain zaps’ - sudden, brief electric shock sensations, often triggered by eye movement.
- Hyperarousal: Anxiety, irritability, panic attacks, restlessness, or even anger outbursts.
But that’s not all. Many people report a feeling like their head is filled with cotton wool, trouble focusing, derealization (feeling detached from reality), or even suicidal thoughts - not because their depression returned, but because their nervous system is in chaos. These symptoms can be intense enough that people rush back to their doctor, convinced they need to restart the medication - and often, they’re right.
Why Some Antidepressants Are Worse Than Others
Not all antidepressants are created equal when it comes to withdrawal. The biggest factor? Half-life - how long the drug stays in your body.
Drugs with short half-lives leave your system fast. That means your brain gets hit with a sudden drop in neurotransmitter levels. That’s why paroxetine (Paxil) and venlafaxine (Effexor) are notorious for causing severe withdrawal. Paroxetine’s half-life is just 21 hours. Venlafaxine’s is under 11 hours. If you miss a dose, your body feels it within hours.
On the other hand, fluoxetine (Prozac) has a half-life of 4 to 6 days. It lingers in your system, acting like a slow drip instead of a sudden stop. That’s why doctors often switch people to fluoxetine if they plan to stop - it makes tapering smoother.
Other classes have their own patterns:
- SSRIs (like sertraline, escitalopram): Brain zaps, dizziness, nausea.
- SNRIs (like venlafaxine, duloxetine): Worse than SSRIs - 47% of users report significant symptoms.
- TCAs (like amitriptyline): Movement issues - tremors, stiff muscles, balance problems.
- MAOIs (like phenelzine): The most dangerous. Can cause agitation, psychosis, catatonia. Requires urgent medical care.

How Long Does It Last?
Most medical guides say symptoms last 1 to 2 weeks. That’s true for many people. But it’s not the whole story.
Community data from patient forums like Surviving Antidepressants - with over 15,000 members - shows 73% of people experience symptoms longer than two weeks. One in four report symptoms lasting over six months. The Royal College of Psychiatrists updated their guidelines in 2022 to acknowledge this: protracted withdrawal is real. Symptoms can drag on for months, sometimes even over a year.
And here’s the catch: the longer you’ve been on the medication, and the faster you stop, the worse and longer it tends to be. That’s why jumping off cold turkey is a recipe for trouble.
Discontinuation vs. Relapse: The Critical Difference
This is where people get misled - and misdiagnosed.
If your depression returns, symptoms build slowly. They take days or weeks to worsen. If you restart the medication, it takes weeks to feel better again.
If you have discontinuation syndrome, symptoms hit fast - often within 24 to 72 hours after missing a dose. And if you take the medication again, they usually vanish within 24 to 72 hours.
That’s the key test. If you feel awful after stopping, and you feel better within a day or two of taking your old dose - it’s withdrawal, not relapse. Mistaking one for the other leads to unnecessary long-term use or, worse, being told you’re just “not coping” when you’re actually going through a physical reaction.
Studies show 38% of cases are misdiagnosed. That’s nearly 4 in 10 people being told they’re depressed again - when they just need time and a slow taper.
How to Manage It: Tapering Is Everything
The best way to avoid discontinuation syndrome? Don’t stop suddenly. Ever.
Medical guidelines agree: taper slowly. For most SSRIs, that means reducing your dose over six to eight weeks. For venlafaxine or other SNRIs, eight weeks or longer is recommended. Some people need months.
Here’s how to do it right:
- Work with your doctor. Never adjust your dose on your own.
- Use a liquid formulation or pill splitter if needed. Exact dosing matters.
- Reduce by 10% to 25% of your current dose every 1 to 2 weeks. Go slower if you feel symptoms.
- Switch to fluoxetine if you’re on a short-half-life drug. It’s a proven strategy.
- Don’t switch to a generic version without checking bioequivalence. Some generics aren’t identical - and that can trigger symptoms.
One study found that tapering over six to eight weeks reduces the risk of severe symptoms by 62%. That’s not a small number. That’s life-changing.
What to Do If You’re Already in Withdrawal
If you’ve already stopped and you’re feeling awful:
- Don’t panic. This is temporary - even if it feels endless.
- Contact your prescriber immediately. Tell them exactly what you’re feeling.
- Reintroducing your original medication - even just a small dose - often brings relief within 72 hours.
- Once symptoms calm down, restart the taper, but slower this time.
Some people find temporary relief with non-medication tools: gentle exercise, good sleep hygiene, omega-3 supplements, magnesium, or even mindfulness practices. These don’t cure it, but they can help your nervous system settle.
High-Risk Situations to Watch For
Some scenarios make discontinuation syndrome more likely - and more dangerous:
- Pregnancy: 41% of pregnant women stop antidepressants without medical advice. That’s a huge risk. Talk to your OB and psychiatrist before making any changes.
- Switching brands: Even switching from one brand to another generic version of the same drug can cause withdrawal. Not all generics are created equal.
- Long-term use: People on antidepressants for more than a year are at higher risk for prolonged symptoms.
- History of withdrawal: If you’ve had this before, you’re more likely to have it again.
And here’s something many doctors don’t mention: stress makes withdrawal worse. If you’re going through a breakup, job loss, or family crisis while tapering, your symptoms will be more intense. Plan your taper for a calm period if you can.
The Bottom Line
Antidepressant discontinuation syndrome isn’t a myth. It’s not a sign you’re broken. It’s a sign your body adapted to the drug - and now it’s trying to readjust. It’s normal. It’s manageable. But it demands respect.
Stopping antidepressants should never be rushed. It’s not a race to be drug-free. It’s a careful, individualized process. Your brain needs time. Your nervous system needs time. And if you’re feeling awful after stopping - you’re not alone. You’re not crazy. You’re experiencing a well-documented physiological response.
The best thing you can do? Talk to your doctor. Ask about tapering. Ask about your medication’s half-life. Ask what to expect. And if you’ve already stopped and you’re suffering - reach out. Help is still possible. Symptoms can fade. Recovery is real - if you take the right steps.




Victoria Stanley
November 24, 2025Just wanted to add that the fluoxetine switch strategy is gold. I was on venlafaxine and went from hellish brain zaps to barely a blip after switching. Took 3 weeks to taper down from the switch dose, and I felt like I’d been given my brain back. Don’t let anyone tell you it’s all in your head - your nervous system remembers.
Vineeta Puri
November 24, 2025It is imperative that individuals be made aware of the physiological nature of discontinuation syndrome. Many are misinformed by primary care providers who lack specialized training in psychopharmacology. The term 'withdrawal' remains stigmatized, yet the clinical evidence is unequivocal. A structured, patient-centered tapering protocol is not optional - it is a medical necessity.
Yvonne Franklin
November 24, 2025Brain zaps are real. I got them bad on sertraline. Stopped cold turkey. Thought I was having a stroke. Took 4 months to settle. Never do that again.
Nikki C
November 25, 2025Been on antidepressants for 8 years. Tried to quit twice. First time I thought I was losing my mind. Second time I tapered over 10 months with liquid citalopram. Still get occasional dizziness if I’m stressed but I’m free. No guilt. No shame. Just science.
Alex Dubrovin
November 26, 2025My doc said I could just stop fluoxetine anytime. I did. Woke up screaming from dreams of falling. Felt like my skull was vibrating. Took 3 days to go back on a quarter dose and the zaps stopped. Never trust a doctor who treats this like a choice
Jacob McConaghy
November 26, 2025Love how this post calls out the generic switch trap. I switched from brand Lexapro to a cheap generic and got hit with dizziness and nausea like I’d been hit by a truck. Took me weeks to figure out it wasn’t relapse - it was the filler in the pill. Pharma doesn’t care if your brain’s on fire as long as you keep buying.
akhilesh jha
November 27, 2025I’ve read this entire post three times. The FINISH mnemonic is brilliant. But I wonder - why isn’t this taught in medical schools? Why do so many doctors still dismiss this as anxiety or depression returning? Is it ignorance? Or is it easier to prescribe than to educate?
Neoma Geoghegan
November 27, 2025Protracted withdrawal is real. 14 months post-discontinuation and I still get sensory overload in fluorescent lights. My neurologist called it ‘neuroplastic recalibration’. I call it surviving. Taper slow. Listen to your body. Not your doctor’s schedule.
Jeff Hicken
November 28, 2025why do people make this so hard?? i just stopped my paxil and yeah i felt weird for a week but i got over it. stop being dramatic. its not a drug addiction its just your body adjusting. jesus
Natashia Luu
November 28, 2025It is regrettable that anecdotal testimonies from online forums are being elevated to the level of clinical evidence. While the phenomenon of discontinuation symptoms is acknowledged, the assertion that 73% experience symptoms beyond two weeks lacks rigorous longitudinal validation. The Royal College’s updated guidelines must be interpreted with caution, particularly when they appear to conflate transient neuroadaptation with chronic pathology. One must not conflate discomfort with disease.