Digoxin-Amiodarone Dose Adjustment Calculator
How to Use This Calculator
Enter patient information below to calculate the appropriate digoxin dose reduction when starting amiodarone. This tool follows clinical guidelines to prevent dangerous toxicity.
Recommended Dose Adjustment
Adjusted Digoxin Dose: mcg/day
Starting amiodarone increases digoxin levels due to interaction with P-glycoprotein. The recommended reduction is based on clinical guidelines to prevent toxicity.
Monitoring Protocol
Next Steps
- Check digoxin levels: 72 hours after starting amiodarone
- Repeat levels: Every 1-2 weeks for first month, then monthly for 3-6 months
- Monitor for toxicity: Nausea, visual changes, heart rhythm issues
- Check potassium: Amiodarone can cause hyperkalemia
Why This Drug Pair Can Be Deadly
Imagine taking two heart medications that have saved your life-until they start working against each other. That’s exactly what happens when digoxin and amiodarone are used together. Both are powerful drugs used to treat irregular heart rhythms, especially atrial fibrillation. But when combined, they can push digoxin levels into the toxic range, turning a life-saving treatment into a life-threatening emergency.
This isn’t a rare glitch. It’s one of the most predictable and dangerous drug interactions in cardiology. Studies show that when amiodarone is added to digoxin therapy, digoxin blood levels can jump by up to 100%. That means a safe dose of digoxin can suddenly become a lethal one. And because digoxin has such a narrow therapeutic window-just 0.5 to 0.9 ng/mL-there’s almost no room for error.
What Happens When These Two Drugs Meet?
Amiodarone doesn’t just sit beside digoxin; it actively interferes with how the body handles it. The main culprit? A protein called P-glycoprotein. This protein normally acts like a gatekeeper, pushing digoxin out of cells so it can be cleared from the body. But amiodarone blocks this gate. The result? Digoxin builds up in the bloodstream like water in a clogged drain.
It’s not just one mechanism. Amiodarone also slows down how quickly the liver breaks down digoxin and reduces kidney clearance. Together, these effects cause digoxin levels to rise sharply-often within days of starting amiodarone. The peak effect doesn’t come right away. It can take one to two weeks. That’s why many doctors miss it. They check levels early, see nothing alarming, and assume it’s safe. But the danger is just getting started.
And here’s the kicker: amiodarone sticks around for months. With a half-life of up to 100 days, even after you stop taking it, the interaction continues. Your digoxin dose may need to stay low for months-or even years.
Who’s at the Highest Risk?
This interaction doesn’t affect everyone the same way. The biggest red flags are age, kidney function, and existing heart conditions.
- Patients over 75 are at significantly higher risk. Their kidneys don’t clear digoxin as well, and their bodies are less able to handle sudden changes.
- Those with chronic kidney disease (eGFR under 60 mL/min) are 3 times more likely to develop toxicity.
- People with heart failure who rely on digoxin for symptom control are especially vulnerable. Stopping digoxin isn’t always an option, so adjusting the dose correctly becomes critical.
A 2021 study found that patients who kept their full digoxin dose when starting amiodarone had a 27% higher chance of dying within 30 days. That’s not a small risk. That’s a medical emergency waiting to happen.
The Clinical Reality: Too Many Mistakes
Despite decades of warnings, this interaction is still mishandled. A 2022 study across 15 U.S. hospitals found that only 44% of patients had their digoxin dose reduced when amiodarone was started. In community hospitals, the error rate jumped to nearly 70%.
Why? Because it’s easy to overlook. Amiodarone is often prescribed in urgent situations-like when a patient goes into rapid atrial fibrillation. Digoxin is already on the chart. The doctor assumes the dose is fine. The nurse administers it. No one checks the interaction.
One case from Massachusetts General Hospital involved a 72-year-old woman who developed dangerous bradycardia and dangerously high potassium levels after starting amiodarone. Her digoxin level was 3.8 ng/mL-nearly four times the upper limit. She ended up in the ICU for four days. She survived. But many don’t.
How to Get It Right: The Proven Protocol
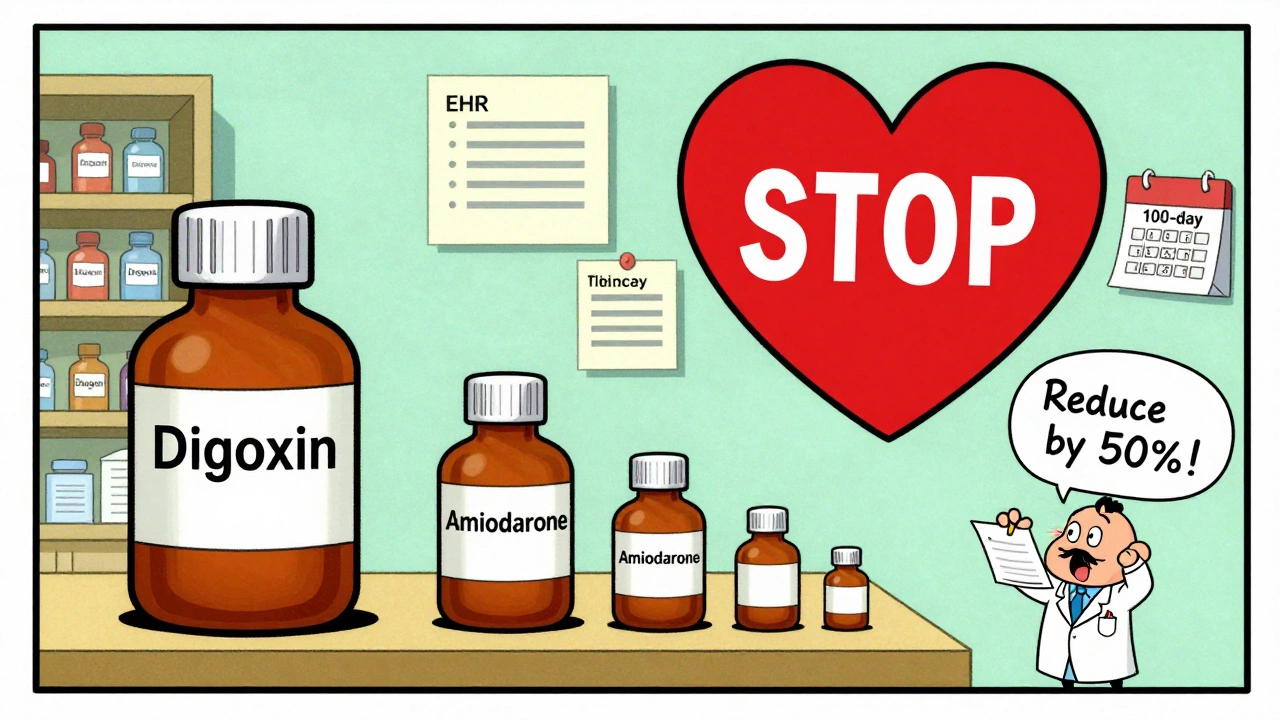
There’s no guesswork here. The fix is simple, well-studied, and backed by decades of evidence:
- Reduce digoxin by 50% at the time amiodarone is started. Don’t wait for lab results. Don’t wait to see symptoms. Start with half the dose immediately.
- Check digoxin levels 72 hours after starting amiodarone. This is non-negotiable. Levels should be drawn before the first amiodarone dose, then again at 72 hours. If levels are still above 0.9 ng/mL, reduce further.
- For patients with kidney impairment (eGFR <50 mL/min), reduce digoxin by 67% (to one-third of the original dose). Their bodies clear digoxin even slower.
- Monitor for symptoms of toxicity: nausea, vomiting, loss of appetite, blurred vision (yellow or green halos), confusion, and new or worsening heart rhythm problems.
- Keep checking levels for weeks-even months. Because amiodarone lingers, digoxin levels can creep up slowly. Don’t assume safety after one normal test.
At the University of Michigan, hospitals implemented a strict protocol: automatic 50% digoxin reduction with amiodarone initiation, plus mandatory lab checks. Toxicity events dropped from 12.3% to just 2.1%.
What About Stopping Amiodarone?
Many assume that once amiodarone is stopped, the risk disappears. It doesn’t. Because amiodarone stays in the body for so long, the interaction can persist for 60 days or more after the last dose. Some patients need to stay on a reduced digoxin dose for months.
Don’t automatically go back to the original digoxin dose. Reassess after 4-6 weeks. Check levels. Watch for signs of rising toxicity. If you increase the dose too soon, you risk triggering toxicity all over again.
Alternatives to Consider
Given the risks, many cardiologists now avoid digoxin altogether in patients who might need amiodarone. Beta-blockers like metoprolol or calcium channel blockers like diltiazem are safer for rate control in atrial fibrillation. They don’t interact with amiodarone and have fewer side effects.
The 2024 European Society of Cardiology guidelines now recommend these alternatives as first-line for patients likely to need amiodarone. Digoxin is no longer the go-to-it’s a last-resort option, especially if amiodarone is on the table.
The Bigger Picture: Why This Matters
This isn’t just about two drugs. It’s about how we manage complex patients with multiple conditions. People with atrial fibrillation often have kidney disease, heart failure, and high blood pressure. They’re on five, six, even ten medications. One small oversight-a missed dose adjustment-can be fatal.
Health systems are starting to catch on. The Veterans Health Administration installed EHR alerts that pop up when both drugs are prescribed together. Since then, digoxin toxicity events have dropped by 41%.
But technology alone won’t fix this. It takes awareness. It takes discipline. It takes remembering that even the most routine decisions-like prescribing a familiar drug-can have deadly consequences if you ignore the interaction.
Final Takeaway: Don’t Guess. Act.
If you’re prescribing amiodarone to someone on digoxin:
- Reduce the digoxin dose by 50%-right away.
- Check the level in 72 hours.
- Keep checking it for weeks.
- Consider switching to a safer alternative if possible.
This interaction is preventable. It’s not mysterious. It’s not rare. It’s predictable. And every time it happens, it’s a failure of the system-not bad luck.
Can digoxin and amiodarone be used together safely?
Yes-but only with strict precautions. Digoxin must be reduced by 50% at the time amiodarone is started, and serum digoxin levels must be checked 72 hours later. For patients with kidney impairment, reduce digoxin by 67%. Even after amiodarone is stopped, the interaction can last for months, so ongoing monitoring is essential.
How long does the digoxin-amiodarone interaction last?
The interaction begins within days of starting amiodarone and peaks at 1-2 weeks. Because amiodarone has an extremely long half-life (up to 100 days), the interaction can persist for 60 days or more after amiodarone is stopped. In some patients, digoxin doses must remain reduced for months.
What are the signs of digoxin toxicity?
Symptoms include nausea, vomiting, loss of appetite, fatigue, confusion, visual disturbances (yellow or green halos around lights), and new or worsening heart rhythm problems like bradycardia or heart block. High potassium levels (hyperkalemia) may also occur. Any of these symptoms in a patient on both drugs require immediate medical evaluation.
Should I stop digoxin if a patient needs amiodarone?
Not necessarily. If digoxin is essential for heart failure control, reduce the dose by 50% and monitor closely. But if the goal is simply rate control for atrial fibrillation, consider switching to a beta-blocker (like metoprolol) or calcium channel blocker (like diltiazem) instead. These are safer alternatives that don’t interact with amiodarone.
Is this interaction still common today?
Yes. Despite decades of awareness, studies show nearly 60% of patients in community settings still receive full-dose digoxin when amiodarone is added. With 1.2 million Americans on both drugs, this remains a major cause of preventable hospitalizations and deaths. EHR alerts and pharmacist-led protocols have helped reduce errors, but gaps remain.
What’s the safest way to monitor this interaction?
Check serum digoxin levels before starting amiodarone, then again at 72 hours. Repeat every 1-2 weeks for the first month, then monthly for 3-6 months. Also monitor kidney function and potassium levels. Don’t rely on symptoms alone-they often appear late. Always assume the interaction is active unless proven otherwise.
What Comes Next?
If you’re managing a patient on both drugs, the next step is simple: audit your practice. Look at your last five patients who received amiodarone. Did you reduce their digoxin? Did you check levels? If not, it’s time to change.
For hospitals and clinics, implement automated alerts in the electronic health record. Train pharmacists to flag these combinations. Create a standard order set that includes the 50% dose reduction as a default.
This interaction has been known for 40 years. We have the tools. We have the data. What we need now is consistent action.



Evelyn Pastrana
December 7, 2025So let me get this straight - we’re still letting doctors prescribe these two together like it’s 1999? 🙄 I mean, I get that medicine moves slow, but this is like using a flip phone in 2024. Half the dose. Check levels. Done. Why is this even a conversation?
om guru
December 8, 2025The clinical protocol outlined is scientifically sound and evidence based. Reduction of digoxin dosage by fifty percent upon initiation of amiodarone is mandatory. Regular serum level monitoring is non negotiable. Patient safety depends on strict adherence to guidelines
Philippa Barraclough
December 9, 2025It's interesting how this interaction has been well documented for decades yet continues to occur with alarming frequency. The pharmacokinetic mechanisms are clear - P-glycoprotein inhibition, reduced hepatic metabolism, and impaired renal clearance all contribute to digoxin accumulation. Yet despite this, the failure rate in clinical practice remains stubbornly high, suggesting systemic issues in both education and workflow design rather than a lack of knowledge.
Tim Tinh
December 10, 2025bro this is wild. i had a grandpa on both of these and no one told us anything. he got super dizzy and started seeing yellow dots. we thought it was just old age. turns out he was one step away from cardiac arrest. please please please tell your docs about this. it’s not hard. just cut the dose in half and check the blood. that’s it.
Olivia Portier
December 11, 2025I’m so glad someone finally laid this out like this. I work in a small clinic and we get so many elderly patients on both meds. We started doing the 50% reduction and mandatory 72hr labs last year - our toxicity cases dropped from 3 a month to zero. It’s not magic. It’s just paying attention. Let’s make this standard everywhere. We can do better.
Tiffany Sowby
December 13, 2025Ugh. Another one of these "medical professionals are clueless" posts. Like we don’t have enough panic content already. Maybe instead of scaring people with 27% mortality stats, we should just fix the broken healthcare system that lets this happen in the first place?
Asset Finance Komrade
December 15, 2025One might posit that this interaction is not merely a pharmacological phenomenon but a metaphysical symptom of our over-reliance on pharmacological solutions to complex physiological states. Amiodarone, a molecule of paradox, lingers like a ghost in the system - a reminder that control is an illusion. 🌌
Jennifer Blandford
December 16, 2025I just cried reading this. My mom almost died from this. She was 78. Her levels were 4.2. They didn’t adjust her digoxin. She was in the ICU for 11 days. I’ve been screaming about this to every doctor I know since. Please. Just. Reduce. The. Dose.
Brianna Black
December 18, 2025This is precisely why I advocate for mandatory clinical decision support in all EHR systems. The fact that this interaction remains undermanaged in 2024 is not a failure of individual clinicians - it is a failure of infrastructure. The data exists. The guidelines are clear. What’s missing is enforcement.
Stacy Tolbert
December 19, 2025I’m just wondering how many people have actually died because of this and no one ever connected the dots. Like… someone goes to the ER with nausea and bradycardia, they treat it as ‘gastro’ or ‘vagal’ and move on. No one checks the med list. No one asks. And then they’re gone. And no one even remembers.
Ryan Brady
December 20, 2025USA still letting this happen? I thought we were the best at medicine. This is why other countries laugh at us. Just cut the dose. It’s not rocket science. 🇺🇸😭
Iris Carmen
December 22, 2025i think this post is kinda overhyped? like yeah the interaction is real but its not like every single person gets toxic. maybe just check levels once in a while instead of panic reducing everything?
Kathy Haverly
December 23, 2025This is why I hate American medicine. You’re all so obsessed with protocols and checklists that you forget patients aren’t algorithms. Sometimes you just need to listen. Maybe the patient’s nausea isn’t toxicity - maybe they’re just stressed. Or maybe you’re just scared to admit you don’t know what you’re doing.
Haley P Law
December 24, 2025I just posted this on my mom’s Facebook group. 17 comments in 10 minutes. Everyone’s like ‘OMG I didn’t know this’ and ‘my aunt died from this’ and ‘why didn’t my doctor tell me?’ I feel like I just started a movement. 💔❤️🩺
Steve Sullivan
December 25, 2025i think the real question is why do we keep using digoxin at all? it’s a 18th century drug with a 21st century risk profile. if we have safer alternatives like diltiazem or beta blockers… why are we still gambling with a drug that can kill you if you blink wrong? maybe we need to stop treating medicine like a hobby and start treating it like a science.