When you're managing bipolar disorder with lithium carbonate, the difference between feeling stable and ending up in the hospital can come down to a tiny number: lithium serum levels. It’s not just about taking the pill-it’s about making sure your body absorbs it the same way every time, especially when switching between generic brands.
Why Lithium Is Different From Other Medications
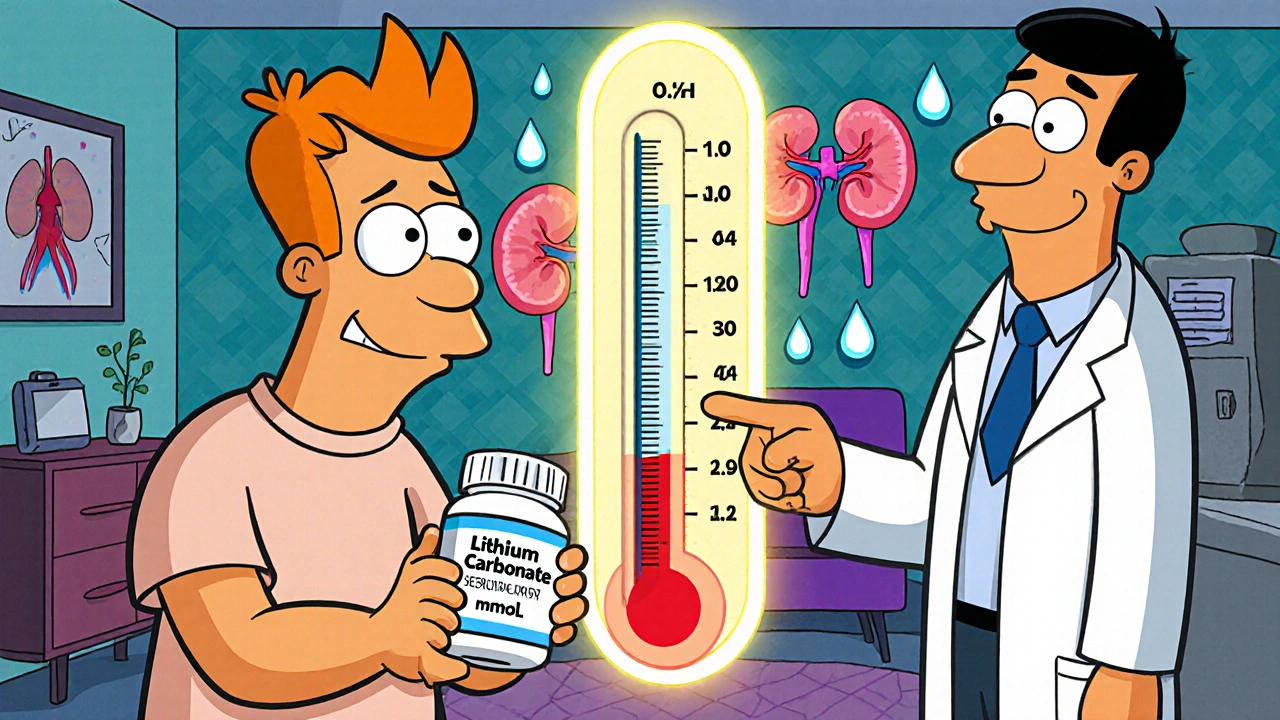
Lithium carbonate isn’t like your usual antidepressant or blood pressure pill. It’s one of the oldest mood stabilizers still in use, dating back to the 1940s when Australian psychiatrist John Cade first noticed its calming effect on agitated guinea pigs. Today, it’s one of the most effective treatments for preventing manic and depressive episodes-and it reduces suicide risk by up to 80% in long-term users. But here’s the catch: lithium has a razor-thin window between working and being dangerous. The therapeutic range? Between 0.6 and 1.2 mmol/L. Go above 1.5 mmol/L, and you risk tremors, confusion, or even seizures. Drop below 0.6, and your mood might start slipping again. That’s what makes it an NTI drug-Narrow Therapeutic Index. One small change in how your body handles the drug can tip the balance.Generics Aren’t Always Interchangeable
You might think all lithium carbonate pills are the same. After all, the FDA says generics must be bioequivalent to the brand. But bioequivalence doesn’t mean identical. It just means the total amount absorbed (AUC) falls within 80-125% of the original. That’s a huge range. Take two common sustained-release generics: Camcolit and Priadel. A 2024 study found that when patients switched from Priadel to Camcolit, their average lithium levels jumped 11%-even though the milligram dose stayed the same. Four patients in that study ended up with levels above 1.3 mmol/L after the switch. One hit 1.88 mmol/L-well into toxic territory. Why? Because the way the drug is released matters. Priadel releases lithium over about 2 hours. Camcolit takes longer. Even small differences in release timing change how much lithium hits your blood at once. That’s why a patient on 900 mg of one brand might need 1,000 mg of another to get the same effect. And it’s not just brand vs. brand. Switching from immediate-release to extended-release can also throw off your levels. Immediate-release tablets peak in 1-2 hours. Extended-release forms peak at 4-5 hours. If you’re used to checking your blood level 12 hours after your last dose (standard for immediate-release), but you’re now on a once-daily extended-release pill, your 12-hour reading will be too low. You might think you’re underdosed and increase your dose-only to overdose later.When to Check Your Lithium Level
Timing isn’t optional. It’s critical. If you’re on immediate-release lithium (taken 2-3 times a day), your blood test should be drawn 12 hours after your last dose. That’s when levels stabilize. If you’re on a once-daily sustained-release formulation, the test should be done 24 hours after your last dose. That’s when the peak has passed and the level reflects true steady-state. Many patients don’t know this. They get tested at random times, or their doctor doesn’t adjust for formulation. The result? Inaccurate readings. A level of 0.7 mmol/L might look perfect-but if it was drawn 6 hours after a sustained-release pill, it’s actually dangerously low. The real level could be 1.0 mmol/L.
What Your Target Level Should Be
There’s no one-size-fits-all target. It depends on your age, your condition, and what kind of lithium you’re taking. For acute mania, most guidelines recommend 0.8-1.0 mmol/L. That’s the range where lithium works best to stop a full-blown episode. For long-term maintenance, the trend is shifting toward lower levels: 0.6-0.8 mmol/L. Why? Because side effects-tremors, weight gain, thyroid problems, kidney strain-add up over time. A 2021 American Psychiatric Association guideline supports this. Lower levels still prevent relapses, with fewer side effects. But here’s the twist: if you’re on a sustained-release formulation, you often need to aim for the higher end of that range. Because the drug releases slowly, your peak is lower. To get the same effect as a higher peak from an immediate-release pill, you need to keep your average level a bit higher. For older adults-especially over 60-doctors often lower the target. Kidneys slow down with age. Lithium clears slower. A level of 0.6 mmol/L in a 25-year-old might be fine. In an 80-year-old, it could be too high. Studies show patients over 80 take nearly 440 mg less lithium per day than younger adults, even when controlling for weight and illness severity.What Else You Need to Monitor
Lithium doesn’t just affect your mood. It affects your whole body.- Thyroid: Up to 15% of people on long-term lithium develop hypothyroidism. Get a TSH test every 6-12 months. If your TSH is above 4.5, you may need thyroid hormone replacement.
- Kidneys: Lithium can cause chronic kidney damage over time. Check your creatinine and eGFR every 3-6 months. The 2022 CANMAT guidelines now recommend using cystatin C instead of creatinine alone-it’s more accurate in older adults and those with low muscle mass.
- Electrolytes: Low sodium (hyponatremia) makes lithium levels rise. If you’re on a low-salt diet, drink less water, or take diuretics, your lithium can spike. Stay consistent with your salt and fluid intake.

What to Do If You Switch Brands
If your pharmacy switches your lithium from one generic to another-without telling you-get your serum level checked within 2 weeks. Don’t wait. Don’t assume it’s fine. Don’t let your doctor say, “It’s the same drug.” It’s not the same in practice. Some clinics now use a simple rule: any change in formulation = new blood test. Even if it’s the same manufacturer but a different batch or packaging. Why? Because small changes in excipients (fillers, binders) can alter absorption. If your level jumps more than 0.2 mmol/L after a switch, your doctor should adjust your dose. And if you feel new tremors, nausea, or confusion-call your doctor immediately. These could be early signs of toxicity.What’s Changing in the Future
Researchers are getting closer to personalized lithium dosing. The International Consortium on Lithium Genetics (ConLiGen) has identified over 30 gene variants that affect how people metabolize lithium. Some people naturally clear it faster. Others hold onto it longer. In the next 5 years, you might see AI tools built into electronic health records that suggest your dose based on your age, weight, kidney function, genetics, and even your recent blood levels. Some hospitals in the U.S. and Europe are already testing these. But for now, the simplest, most powerful tool is still the blood test. No algorithm replaces knowing your actual serum level.Final Thought: Trust the Number, Not the Brand
Lithium carbonate generics are cost-effective. They save patients and healthcare systems millions. But they’re not interchangeable. The brand name doesn’t matter as much as the number on your lab report. If you’re on lithium, make sure:- You know which formulation you’re on (immediate or extended-release)
- You know when to get your blood drawn (12 or 24 hours after your last dose)
- You get tested after every brand or formulation change
- You track your thyroid and kidney function regularly



Maria Romina Aguilar
November 29, 2025So... I switched from Priadel to Camcolit last month, and I didn't get tested. I just figured, 'it's lithium, right?' Now I'm shaky at 3am and my hands won't hold a coffee cup. I didn't think it was a big deal until I Googled 'lithium tremors' and found this post. I'm getting my blood drawn tomorrow. I'm terrified.
Brandon Trevino
November 30, 2025The data is unambiguous. Bioequivalence standards for NTI drugs are statistically inadequate and clinically reckless. The FDA's 80-125% AUC window permits pharmacokinetic variance that exceeds therapeutic safety margins. This is not a regulatory oversight-it is systemic negligence. Every generic substitution without therapeutic drug monitoring constitutes an act of medical malpractice by omission.
Denise Wiley
December 1, 2025Thank you for writing this. I've been on lithium for 12 years and no one ever told me about the 24-hour rule for extended-release. I've been getting tested at 12 hours my whole life. No wonder my levels always looked 'fine' but I still felt off. I'm going to ask my psych to change it. Also, I cried reading this. I'm not alone. 💛
Hannah Magera
December 3, 2025I'm new to lithium and this post helped me so much. I didn't know about thyroid or kidney checks. My doctor just said 'take this pill.' I didn't know I needed to track anything else. Can someone explain what eGFR is? I looked it up but got confused. Thanks for being patient with beginners.
Austin Simko
December 4, 2025They're poisoning us. Big Pharma controls the generics. The FDA is bought. Watch the levels drop after switch. Then they blame you for relapsing.
Nicola Mari
December 5, 2025It's appalling that patients are treated like lab rats with this drug. You're not supposed to be a guinea pig. You're supposed to be a person. And yet, we're handed pills like they're candy, and told to hope for the best. It's not just negligence-it's cruelty dressed up as cost-saving.
Sam txf
December 5, 2025Let me guess-you're one of those people who thinks 'it's just lithium' and doesn't realize this is the most dangerous mood stabilizer ever invented. You think your doc is doing you a favor? Nah. They're just lazy. You need to be your own advocate. Or die trying.
Michael Segbawu
December 6, 2025I switched to a new generic last year and got sick as a dog for two weeks. My doctor said it was 'just adjustment' and gave me more pills. I almost went to the ER. Now I only take the brand name even though it costs 3x. Screw the system. My life is worth more than their savings.
Aarti Ray
December 7, 2025I live in India and we dont have brand name lithium here. Only generics. My doctor here says all are same. But I feel different when I get different batch. I asked for test but they said its expensive. I wish I knew what you wrote earlier. Thank you for sharing. I will try to get test next month.
Alexander Rolsen
December 9, 2025Who the hell lets a patient switch generics without a level check? That's not medical practice-that's Russian roulette with a loaded gun. And you know who pays the price? The patient. The system doesn't care. They'll write you another script, another blood test, another excuse. But you're the one who wakes up trembling, nauseated, wondering if today's the day you don't make it.
Leah Doyle
December 10, 2025This is the most helpful thing I've read in years. I've been on lithium for 8 years and never knew about the 12 vs 24 hour thing. I've been getting tested wrong the whole time. I'm going to print this out and give it to my doctor. Thank you so much. 🙏
Alexis Mendoza
December 10, 2025It's interesting how something so simple-a blood test-can be so revolutionary. We live in a world obsessed with complex algorithms and AI, but the most powerful tool we have is still the humble lab report. Maybe the answer isn't more technology, but more attention. More care. More listening to what the numbers say, not just what the label says.