Most people with chronic kidney disease (CKD) don’t know they have it-until it’s too late. By the time symptoms like fatigue, swelling, or foamy urine show up, the kidneys have already lost half their function. And yet, if caught early, CKD progression can be slowed or even stopped. The key isn’t waiting for symptoms. It’s knowing the two simple tests that reveal kidney damage long before it’s obvious.
What Chronic Kidney Disease Really Means
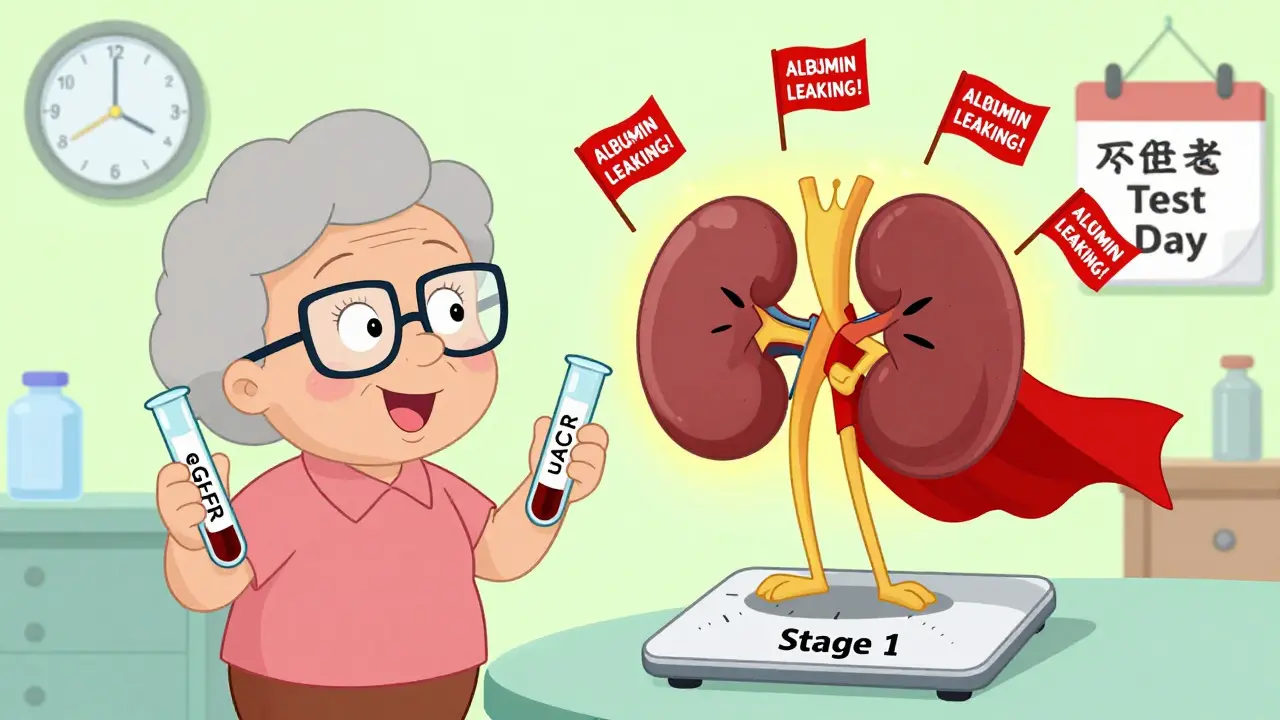
Chronic kidney disease isn’t just about low kidney function. It’s about damage that lasts three months or longer. This damage can show up in two ways: either your kidneys aren’t filtering blood well (measured by eGFR), or they’re leaking protein into your urine (measured by uACR). You need both to be abnormal to get a true CKD diagnosis. The old way of checking kidneys? Just a blood test for creatinine. That’s not enough. Creatinine levels vary wildly based on muscle mass, age, race, and even what you ate for dinner. A healthy 70-year-old woman with low muscle mass might have a normal creatinine-but still have damaged kidneys. That’s why 30-40% of early CKD cases were missed for years. Now, the standard is clear: eGFR and uACR. Together, they tell the full story. eGFR estimates how well your kidneys filter waste. uACR measures how much albumin-a type of protein-is leaking out. If uACR is 30 mg/g or higher, your kidneys are leaking. That’s a red flag, even if your eGFR is still in the normal range.The 5 Stages of CKD-And Why Stage 1 and 2 Matter Most
CKD is broken into five stages, based on eGFR and the presence of kidney damage:- Stage 1: eGFR ≥90, but uACR ≥30 mg/g. Kidneys are working fine, but damage is present.
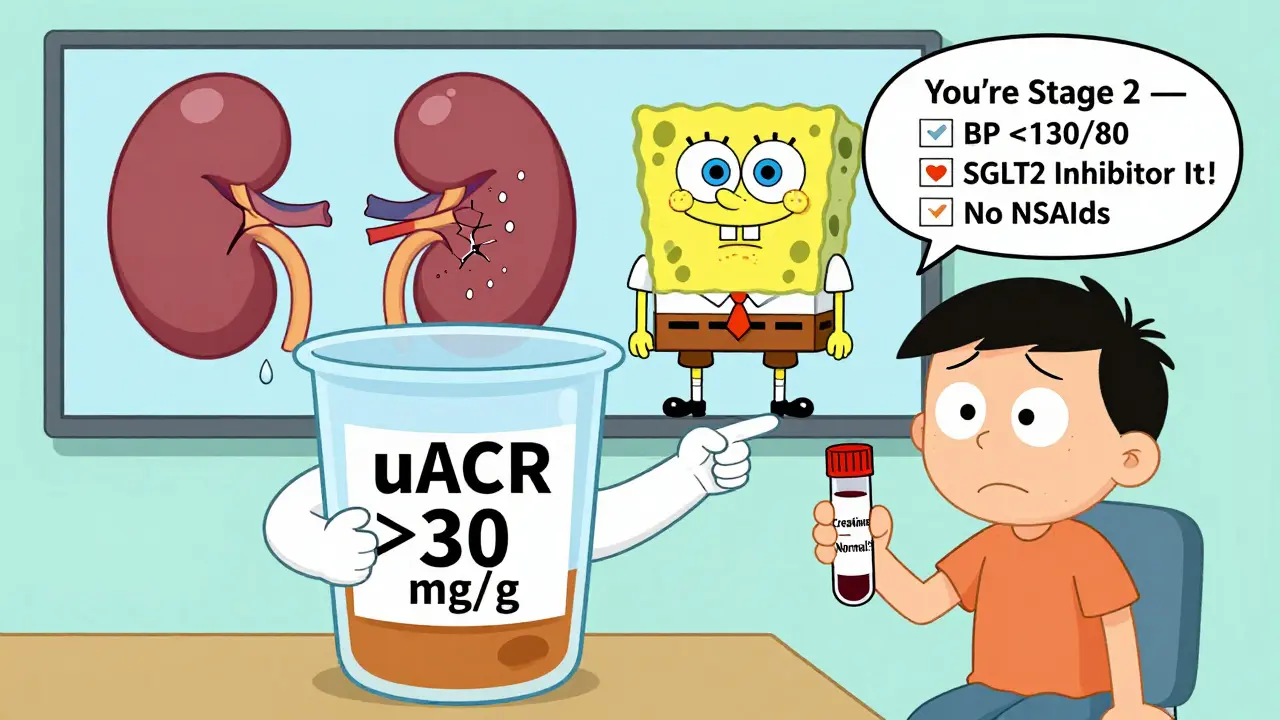
- Stage 2: eGFR 60-89, uACR ≥30 mg/g. Slight decline, but still early.
- Stage 3a: eGFR 45-59. Mild to moderate loss.
- Stage 3b: eGFR 30-44. Moderate to severe loss.
- Stage 4: eGFR 15-29. Severe loss.
- Stage 5: eGFR <15. Kidney failure. Dialysis or transplant needed.
Who Needs Screening-and How Often?
You don’t need to be sick to get tested. If you have any of these, you’re at risk:- Diabetes (type 1 or 2)
- High blood pressure
- Heart disease
- Family history of kidney failure
- African American, Native American, or Hispanic heritage
- Obesity
- Chronic use of NSAIDs (like ibuprofen or naproxen)
- Age 60 or older
- If you have diabetes: Get tested every year, starting at diagnosis for type 2, or five years after diagnosis for type 1.
- If you have high blood pressure: Get both tests at least once a year.
- If you’re over 60 with no known risk: Ask your doctor. Many people in this group are undiagnosed.
The Two Tests That Save Kidneys
eGFR (estimated Glomerular Filtration Rate) This comes from a simple blood test. It uses your creatinine level, age, sex, and race to estimate how much blood your kidneys filter each minute. The current gold standard is the CKD-EPI equation, updated in 2009. But here’s the catch: creatinine can be misleading. If your eGFR is between 45 and 59-and you have no known kidney disease or protein in your urine-your doctor should consider a cystatin C test. This is a more accurate marker of kidney function, especially if your muscle mass is low or you’re older. It doesn’t depend on diet or muscle size. uACR (urine Albumin-to-Creatinine Ratio) This test uses a single urine sample. No special collection needed. The lab measures how much albumin is in your urine compared to creatinine. If it’s 30 mg/g or higher, you have albuminuria. That means your kidney filters are leaking. It’s one of the earliest signs of damage. The best sample? First-morning urine. It’s more concentrated and gives the clearest signal. Avoid testing after intense exercise, infection, or fever-those can cause false spikes.What Happens After Diagnosis?
If you’re diagnosed at stage 1 or 2, you’re not doomed. You’re in control. Here’s what works:- Control blood pressure: Target <130/80 mmHg. The SPRINT trial showed this cuts progression risk by 27% compared to the old target of <140/90.
- Use SGLT2 inhibitors: Originally diabetes drugs, these (like empagliflozin or dapagliflozin) now have FDA approval for CKD-even without diabetes. The CREDENCE trial showed they reduce progression to kidney failure by 32%.
- Reduce salt: Aim for under 2,300 mg a day. High salt raises blood pressure and strains kidneys.
- Stop NSAIDs: Regular ibuprofen or naproxen use can damage kidneys over time. Use acetaminophen instead if you need pain relief.
- Quit smoking: Smoking narrows blood vessels, including those in the kidneys.
- Work with a dietitian: A low-protein, low-phosphorus, low-potassium diet can ease the burden on your kidneys.
Why Most People Still Get Missed
Despite clear guidelines, most people with early CKD go undiagnosed. Why?- Doctors order only creatinine, not uACR.
- EHR systems don’t remind providers to test both.
- Patients don’t know to ask.
- Some think “normal creatinine” means healthy kidneys.

The Future: AI, Point-of-Care Tests, and Policy Changes
The tools are getting better. In May 2023, the FDA cleared the first AI tool-NephroSight by Renalytix-that analyzes 32 data points (blood pressure, age, lab results, medications) to predict who’s at risk of CKD before their eGFR drops. It’s already being used in some VA hospitals. By 2025, point-of-care uACR devices will be available in clinics. No lab wait. Results in 10 minutes. That could boost screening rates by 40%. And policy is catching up. The Biden administration’s 2023 Executive Order on Kidney Health includes $150 million to make dual-testing mandatory in federally funded clinics by 2026. That could catch 1.2 million new cases. Japan and Australia have had national screening programs for years. Their rates of kidney failure dropped 18-22% over 15 years. The U.S. can do the same.What You Can Do Today
If you’re at risk:- Ask your doctor for both an eGFR and a uACR test.
- If you’re diabetic or hypertensive, get tested every year-no exceptions.
- Don’t ignore protein in urine. It’s not just a “minor issue.”
- If you’re diagnosed with stage 1 or 2, don’t panic. Act.
- Get a copy of your results. Know your numbers.
Can you have chronic kidney disease with normal creatinine?
Yes. Creatinine alone misses up to 40% of early kidney damage. You can have normal creatinine but still have protein in your urine (uACR ≥30 mg/g), which is a sign of kidney damage. That’s why both tests are required for diagnosis.
Is CKD reversible?
In stages 1 and 2, yes-progression can be stopped or significantly slowed. Medications like SGLT2 inhibitors, strict blood pressure control, and lifestyle changes can preserve kidney function for decades. Once you reach stage 3 or higher, the damage becomes harder to reverse, but further decline can still be slowed.
Do I need a kidney biopsy if I’m diagnosed with CKD?
No, not usually. Most cases of CKD are caused by diabetes or high blood pressure and don’t require a biopsy. Biopsies are only done when the cause is unclear, or if there’s sudden worsening, heavy proteinuria, or blood in the urine without explanation. Less than 2% of CKD patients need one.
Can I prevent CKD if I have diabetes?
Absolutely. Tight blood sugar control reduces kidney damage risk by 30-50%. Combined with blood pressure control and SGLT2 inhibitors, many people with diabetes never develop kidney disease. Annual uACR and eGFR testing is the key to catching early signs before damage becomes permanent.
Why does race matter in eGFR calculations?
Historically, eGFR formulas added a “race correction” for Black patients, assuming they had higher muscle mass. But this led to underdiagnosis. Newer formulas are moving away from race, and early data shows removing it could increase early detection in Black patients by 12%. The goal is accuracy, not assumptions.
Are over-the-counter painkillers dangerous for kidneys?
Regular use of NSAIDs like ibuprofen, naproxen, or aspirin can reduce blood flow to the kidneys and cause damage over time, especially if you already have reduced kidney function. Acetaminophen (Tylenol) is safer for kidneys, but always check with your doctor if you’re taking it daily.
Can I live a normal life with early-stage CKD?
Yes. Many people with stage 1 or 2 CKD live full, active lives for decades. The key is early detection and consistent management-controlling blood pressure, avoiding kidney-toxic drugs, eating right, and getting regular checkups. It’s not a death sentence-it’s a call to take charge.




Nicola George
December 27, 2025So let me get this straight - we’re supposed to believe that two blood tests are the magic bullet for a disease that’s been quietly killing people for decades? Yeah, right. I’ve seen too many folks get flagged for ‘early CKD’ only to find out their ‘protein leak’ was just dehydration from a marathon run or their eGFR got skewed because they did 200 squats before the lab visit. Stop selling fear as medicine.
James Bowers
December 28, 2025It is imperative to underscore that the diagnostic criteria for chronic kidney disease, as delineated by the National Kidney Foundation’s Kidney Disease: Improving Global Outcomes (KDIGO) guidelines, necessitate the concurrent assessment of both estimated glomerular filtration rate (eGFR) and urine albumin-to-creatinine ratio (uACR). Relying solely upon serum creatinine constitutes a clinically inadequate approach, as it fails to account for inter-individual variability in muscle mass, age-related nephron loss, and dietary influences. Consequently, the omission of uACR in routine screening protocols has resulted in a substantial proportion of early-stage pathology being overlooked.
Janice Holmes
December 29, 2025MY KIDNEYS ARE CRYING IN THE CORNER RIGHT NOW 😭
They’ve been leaking albumin like a busted faucet since 2021 and NO ONE TOLD ME?!?!
My doctor said my creatinine was ‘fine’ - FINE?!? That’s like saying your house isn’t on fire because the smoke alarm hasn’t screamed yet!
uACR is the REAL hero here - it’s the silent sentinel, the canary in the coal mine, the whisper that says ‘hey dumbass, you’ve been drinking soda like it’s water for 12 years’!
They should test EVERYONE over 40 - like a mandatory wellness check, right after your colonoscopy and before your annual ‘why are you still single?’ interrogation.
Andrew Gurung
December 30, 2025Ugh. Another ‘medical authority’ pushing another ‘simple test’ narrative. 🙄
Of course it’s not just creatinine - but guess what? The real problem is Big Pharma pushing ‘early detection’ so they can sell you expensive meds for 30 years before you even feel sick.
Meanwhile, your kidneys are fine - you just need to stop eating processed junk and start walking. But hey, let’s monetize your fear with another lab bill. 💸
Also, ‘Stage 1 CKD’? That’s not a diagnosis - it’s a marketing ploy. 😒
Olivia Goolsby
December 31, 2025Have you ever stopped to think… that these ‘eGFR’ and ‘uACR’ numbers… are they even real?!? Or are they just algorithms cooked up by corporate labs to justify endless testing?!? I mean - who calculates eGFR? Who owns the algorithm?!? And why does it suddenly change if you’re Black or white?!? And what if your ‘protein leak’ is just from your protein shake?!? What if the ‘30 mg/g’ threshold was pulled out of a corporate PowerPoint deck?!? And what if the real reason they don’t want you to just check creatinine… is because they don’t want you to know that your kidneys are fine… but your blood pressure meds are making you dizzy?!? And what if… the whole system… is designed… to keep you scared… and buying… and testing… and paying… for the rest of your life?!?!
Will Neitzer
January 1, 2026While the diagnostic framework for chronic kidney disease has evolved significantly over the past decade, the clinical imperative remains unchanged: early identification of structural or functional renal injury enables timely intervention that demonstrably delays progression to end-stage renal disease. The integration of uACR into routine screening protocols has been validated in multiple longitudinal cohort studies, including the Atherosclerosis Risk in Communities (ARIC) and the Chronic Renal Insufficiency Cohort (CRIC) studies. These data unequivocally demonstrate that individuals with isolated albuminuria - even with preserved eGFR - exhibit significantly higher rates of cardiovascular morbidity and renal decline over time. Therefore, dismissing early-stage CKD as ‘preclinical’ or ‘non-actionable’ is not merely inaccurate - it is clinically negligent.
Chris Garcia
January 2, 2026In my village back in Nigeria, we used to say: ‘The body speaks before it screams.’
Our grandmothers didn’t have eGFR or uACR - but they knew when someone’s feet swelled in the morning, or when their urine looked like foam from a beer bottle left in the sun.
Today, we have science - but we’ve lost the wisdom to listen.
These tests aren’t just numbers - they’re the language of your body begging you to slow down.
Don’t wait for the scream.
Check the whisper.
And if you’re eating salt like it’s candy, drinking soda like it’s tea, and sitting like a statue all day… no test will save you.
Change your life - before the machine tells you it’s too late.
Nikki Thames
January 2, 2026It is profoundly disconcerting to observe the persistent public misconception that kidney health is merely a function of hydration or dietary supplements. The notion that one can ‘detox’ their kidneys with lemon water or green tea is not only scientifically baseless - it is dangerously misleading. The pathophysiology of chronic kidney disease is inexorably tied to metabolic syndrome, hypertension, and systemic inflammation - conditions that are not remediated by wellness trends, but rather require sustained, evidence-based medical management. To reduce this complex, multifactorial pathology to a single biomarker or a ‘simple test’ is to trivialize the lived experience of millions who endure progressive organ failure - often in silence - due to systemic neglect, not ignorance.