Pharmacy Labels: What They Mean and How to Read Them Safely
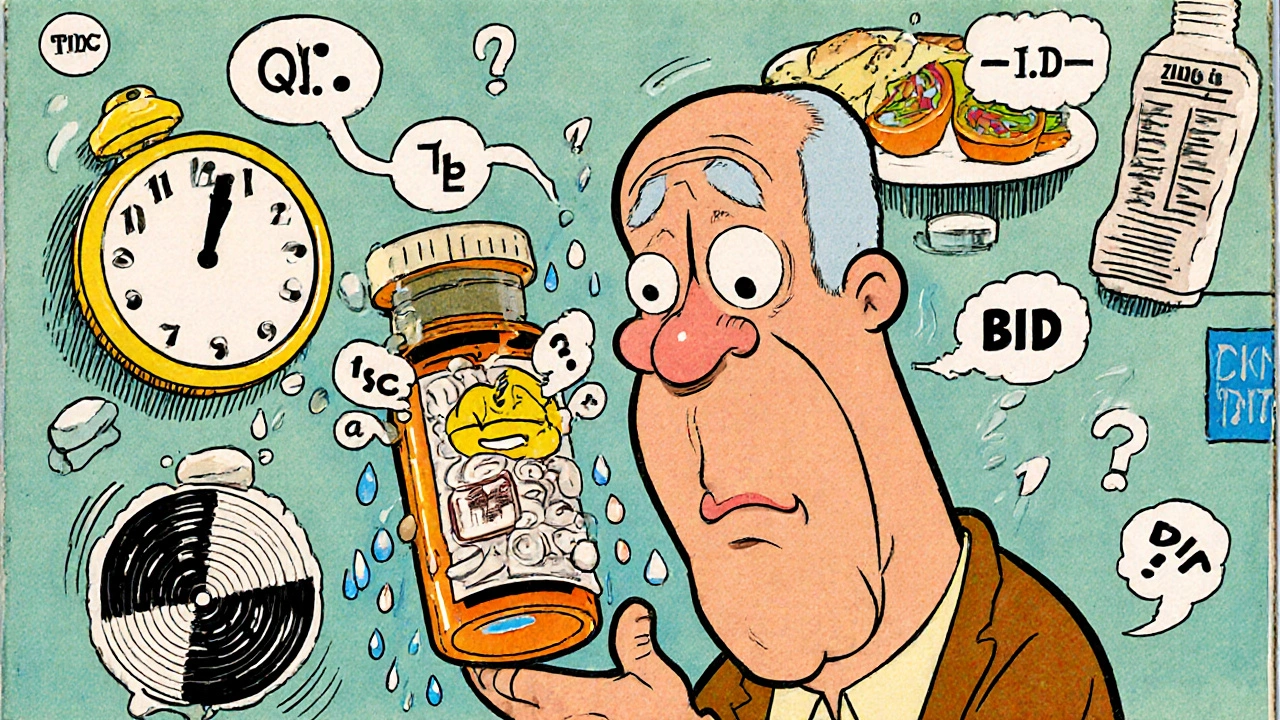
When you pick up a prescription, the pharmacy labels, the printed information on prescription bottles that tell you how to take the drug, its risks, and who made it. Also known as medication labels, they’re your first and last line of defense against mistakes. These aren’t just small pieces of paper—they’re legal documents with life-or-death details. Yet most people glance at them like ads, missing the warnings, timing instructions, and interaction alerts hidden in plain sight.
Behind every pharmacy label is a system built by the FDA drug labels, official, standardized documents that drug manufacturers must submit to the U.S. Food and Drug Administration, detailing every known effect, warning, and dosage. These labels pull directly from the FDA’s SPL documents, Structured Product Labeling files that organize drug data into machine-readable formats used by pharmacies and insurers. If you’ve ever searched for drug info on FDALabel, you’ve seen the source material behind the label on your bottle. But what’s on the bottle? It’s a distilled version—often missing the fine print about food interactions, genetic risks, or how it affects kidney function. That’s why reading it carefully matters. A label might say "take once daily," but if your drug is metabolized by CYP2C19 (like clopidogrel), and you’re also on omeprazole, that single daily dose could be dangerously ineffective. The label won’t spell that out.
Pharmacy labels also don’t tell you about formulary changes, insurance restrictions, or generic substitutions that might alter how your drug works. That’s why the same pill from two different pharmacies can feel different—sometimes due to inactive ingredients, sometimes due to bioequivalence gaps. Generic drugs are supposed to be identical, but when they fail, it’s often because the label didn’t warn you about the specific formulation. And if you’re on multiple meds, the label won’t flag interactions with over-the-counter cold meds, herbal supplements, or even grapefruit juice—like with simvastatin. That’s where you need to dig deeper.
People with G6PD deficiency, seniors on NSAIDs like mefenamic acid, or those with heart conditions on stimulants for ADHD all face hidden risks that pharmacy labels barely hint at. The label says "may cause dizziness." But for someone on tamsulosin, that dizziness could mean a fall. For someone on nitrofurantoin, it could mean hemolytic anemia. The label doesn’t say: "If you have this rare condition, don’t take this." You have to know to ask.
That’s why the posts below give you the real breakdowns—not just what’s on the label, but what’s missing. You’ll find guides on how to decode FDA drug labels like a pro, spot dangerous interactions hidden in plain sight, and understand why your generic might not work the same as the brand. You’ll learn how to ask for the full prescribing information, how to check for black box warnings, and what to do when the label contradicts what your doctor said. These aren’t theoretical tips. They’re the kind of knowledge that keeps people out of the ER. Read them before your next refill.