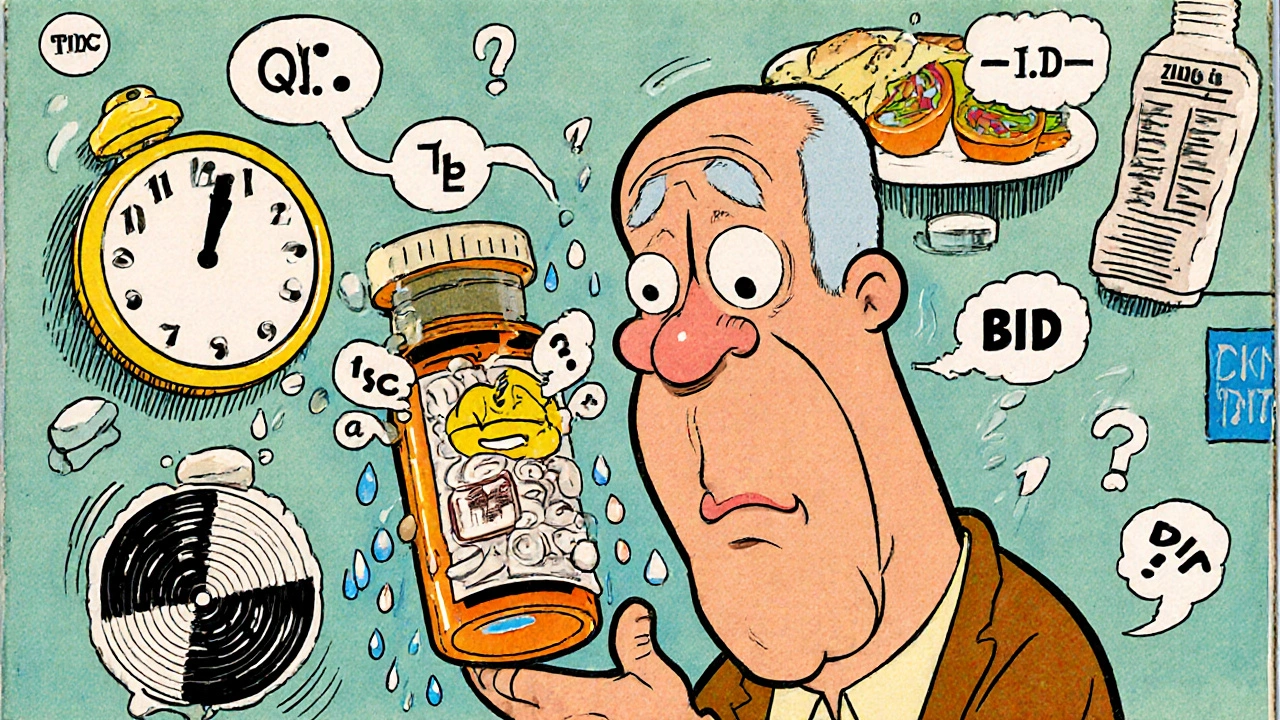
Every year, millions of people in the U.S. take their medication wrong-not because they’re careless, but because the label on the bottle doesn’t make sense. You might think, "I can read, so I’ll figure it out." But even people with college degrees get confused. A pill bottle might say "take every 6 hours"-but does that mean 4 times a day? Or 3 times? What if it says "take with food"? Does that mean right after a meal? Or just anytime you eat something? These aren’t trick questions. They’re real-life mistakes that land people in the emergency room.
Why Prescription Labels Are So Hard to Understand
Pharmacy labels weren’t designed with real people in mind. They were built for efficiency, not clarity. You’ll see phrases like "q.i.d." or "PO" or "BID." These aren’t just confusing-they’re outdated. The average person doesn’t know Latin abbreviations. And even when they’re written out in plain English, the wording is often too complex. A 2006 study found that 46% of patients misunderstood at least one instruction on their prescription label. That’s nearly half of all people filling prescriptions. The problem gets worse for older adults, people with low health literacy, or those who speak languages other than English. Labels often use words like "administer," "ingest," or "titrate." These aren’t everyday words. The FDA says prescription labels should be written at a 6th-grade reading level. But many are written at an 8th- or 10th-grade level. That’s 12.9 times more likely to be misunderstood. And it’s not just the words. The layout matters too. Some labels cram in too much info. Others use tiny fonts. Some don’t even include the most important thing: when to take the medicine. Instead of saying "Take one tablet at 8 a.m. and another at 8 p.m.," they say "Take twice daily." That’s not helpful. People don’t know if that means morning and night-or 12 hours apart, or 6 hours apart.What People Actually Get Wrong
Here are the most common misunderstandings, based on real patient reports and studies:- "Take once daily" vs. "Take once" - Some patients think "take once" means take it one time total, not every day. They skip doses for days, then panic when symptoms return.
- "Take every 4 to 6 hours" - Many people interpret this as "take it every 4 hours," leading to overdose. Others think it means "take it when you feel pain," which can lead to underuse.
- "Take with food" - Some patients think it means "take instead of food." Others take it on an empty stomach because they didn’t eat at the time they were supposed to.
- "Take at bedtime" - Some people take it right before they go to sleep, even if the medicine needs to be taken 2 hours before bed. Others assume it means "when you’re ready to sleep," which could be 2 a.m.
- "Take as needed" - This one’s tricky. Does "as needed" mean every time you feel a little pain? Or only when it’s severe? Many patients overuse or underuse these meds because the line isn’t clear.
What Makes a Label Work?
Good labels don’t rely on jargon. They don’t assume you know what "BID" means. They use simple, direct language. Here’s what works:- Use active voice: "Take 1 tablet by mouth twice a day" - not "One tablet should be taken orally twice daily."
- Specify times: "Take one tablet at 8 a.m. and one at 8 p.m." - not "twice daily."
- Use icons: A clock icon next to "take at bedtime" helps. A plate icon next to "take with food" helps even more.
- Keep it short: No more than two steps. If the instruction needs more, break it into separate lines.
- Use large font: At least 12-point type. If you’re over 65, you need bigger text.
- Include warnings clearly: "Do not drink alcohol" should not be buried under a tiny symbol. It should be in bold, plain language.
How Pharmacists Can Help (And How They’re Starting To)
Pharmacists aren’t just dispensing pills. They’re safety checkpoints. But most don’t have time to explain every label. That’s changing. The "Teach-Back" method is working. Instead of just saying, "Do you understand?" pharmacists ask patients to repeat the instructions in their own words. "Can you tell me when and how you’ll take this?" If the patient says, "I’ll take it when I feel dizzy," the pharmacist knows there’s a problem-and can fix it right then. Some states, like California, now require pharmacy technicians to get training in health literacy. That’s led to a 33% drop in label-related errors. And it’s not expensive. It takes about 8 hours of training per staff member. Pharmacies are also starting to offer:- Large-print labels (available at 89% of major chains)
- Labels in Spanish and other languages (though only 12% of pharmacies offer them, despite 41 million Spanish speakers in the U.S.)
- QR codes that link to video instructions (new as of January 2025)
- Voice-enabled labels through apps like Amazon Pharmacy’s new feature
What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s how to protect yourself:- Ask the pharmacist: "Can you explain how to take this in plain English?" Don’t be shy. They’re there to help.
- Ask for a written copy with times: "Can you write down when I should take it? Like 8 a.m. and 8 p.m.?"
- Request large-print labels if you have trouble reading small text.
- Use your phone: Take a photo of the label and send it to a family member or friend. Ask them to read it back to you.
- Use free tools: The GoodRx "Label Lens" app lets you scan your label and gets a simplified version in seconds. It’s 89% accurate.
- Check the FDA’s website for standardized icons. If you see a symbol you don’t recognize, ask about it.

The Bigger Picture: Why This Matters
Medication errors from bad labels cause 1.3 million emergency room visits every year. That’s more than car accidents. And 350,000 of those lead to hospital stays. The cost? Over $200 billion annually. It’s not just about money. It’s about safety. People die because they took too much. Or too little. Or at the wrong time. And it’s not because they’re stupid. It’s because the system failed them. New rules are coming. By 2025, 17 states will require health-literate labels. The FDA is considering federal standards. And technology is catching up. But until then, you have to be your own advocate.What’s Next?
If you’re on multiple medications, ask your pharmacist for a medication review. They can check for interactions and make sure every label makes sense. If you’re caring for an older relative, sit with them when they fill a new prescription. Read the label together. Ask questions. Don’t assume they understand. This isn’t just a pharmacy problem. It’s a public health problem. And it’s solvable. But only if we all speak up.What should I do if I don’t understand my prescription label?
Don’t guess. Call your pharmacy or ask your pharmacist directly. Say, "I’m not sure what this means. Can you explain it in simple terms?" You can also ask for a written version with specific times (like 8 a.m. and 8 p.m.) instead of "twice daily." Many pharmacies now offer large-print labels or labels in other languages-just ask.
Are pharmacy labels required to be easy to read?
No, not yet by federal law. But the U.S. Pharmacopeia (USP) has created clear standards called Chapter <17>, which recommend plain language, large font, and specific timing instructions. Many chain pharmacies like CVS and Walgreens follow these, but independent pharmacies often don’t. Some states are passing laws to require them by 2025, but there’s no nationwide rule yet.
What do symbols like a plate or clock mean on my label?
These are visual aids meant to help you remember instructions. A plate icon usually means "take with food." A clock icon means "take at a specific time," like bedtime. But not all symbols are standardized. The FDA has tested common icons and found that 68% of patients still misunderstand them. If you’re unsure, always ask your pharmacist to confirm what the symbol means.
Can I get my prescription label in Spanish or another language?
Some pharmacies offer translated labels, but it’s not common. Only about 12% of U.S. pharmacies provide labels in Spanish, even though over 41 million people in the U.S. speak it. You have to ask. Many chains will print a translated version if you request it. If your pharmacy doesn’t offer it, ask for a printed English version and take it to a translator or use a free app like Google Translate to help.
Is it safe to take a medication if the label looks different from last time?
Never assume it’s the same. Even small changes in wording, font size, or icon placement can mean a different instruction. Always compare the new label to the old one. If anything looks different-dose, frequency, timing-ask the pharmacist. It could be a new batch, a different generic version, or a mistake. Better safe than sorry.



Ellen Sales
November 26, 2025God, I just had to explain to my mom why her blood pressure med wasn't working-she thought 'twice daily' meant morning and lunch, not morning and bedtime. She's 72. She didn't even know what 'PO' stood for. This isn't just confusing-it's dangerous.
And don't get me started on the tiny font. I had to use my phone's magnifier just to read the dosage. Who designed this? A robot with no empathy?
Jennifer Griffith
November 27, 2025lol i once took my antibiotic 8 times a day bc i thought 'q6h' meant 6 hours apart and i counted 24/6=4 but then i forgot if it was 4 or 8 so i just did it every 3 hrs. turned out i was fine but my stomach hated me for a week. pharmacy people are so lazy.
Pallab Dasgupta
November 28, 2025Bro this is why India’s healthcare system is so messed up too. We get prescriptions in English with Latin abbreviations and no one explains them. My uncle took his diabetes med at night because it said 'take once daily'-he thought it meant once total. He ended up in ICU. This isn’t a U.S. problem. It’s a global failure.
And don’t even get me started on how pharmacies in small towns just hand you the bottle and say 'you’re good' and walk away. No wonder people die.
Kimberley Chronicle
November 29, 2025The USP Chapter 1101 standards are a godsend, but adoption is patchy because of cost and inertia. Pharmacists are overworked, underpaid, and often lack the training to implement health literacy protocols. The real bottleneck isn’t the label-it’s the system that treats patient education as an afterthought.
QR codes? Brilliant. But only if the video is subtitled, translated, and under 90 seconds. Otherwise, it’s performative tech. We need standardized, ADA-compliant, multilingual, icon-driven labeling-mandatory, not optional.
Emily Craig
November 30, 2025So let me get this straight-we spend billions on drugs but won’t spend $0.02 on bigger fonts or clearer instructions? Amazing. The pharmaceutical industry makes billions off us, then blames us for not being able to decode their medieval hieroglyphics.
Next they’ll say we're dumb for not knowing what 'BID' means. Nah. It’s the system that’s broken. And they know it.
Karen Willie
December 1, 2025I work at a community clinic and we’ve started printing simple instructions on sticky notes and taping them to the bottle. 'Take 1 pill when you wake up. Take 1 pill before bed.' No jargon. No Latin. Just clear.
Patients smile. They say 'this makes sense now.' It takes 30 seconds. Why isn’t this standard everywhere?
Leisha Haynes
December 2, 2025My grandma’s label said 'take with food' so she took it with a bag of chips at 2am. She didn’t think it counted as 'food.' I laughed until I cried. Then I cried because she almost got hospitalized.
Pharmacies need to stop acting like we’re all PhDs who read medical journals. We’re not. We’re tired people trying not to die.
Srikanth BH
December 2, 2025This is so true. I’ve seen this in rural India too-people take half doses because they think 'twice daily' means two pills total, not every day. No one teaches them. No one checks. And when they get sick, they blame themselves.
But here’s the good part: my local pharmacy now has a little card with icons. A sun for morning, a moon for night, a plate for food. Simple. I wish every pharmacy had this. It’s not hard. Just human.
fiona collins
December 4, 2025I just asked for a large-print label. They gave it to me. No fuss. It’s that easy.
Shivam Goel
December 4, 2025Let’s not pretend this is about literacy. It’s about profit. Pharmacies don’t want to spend money redesigning labels. They’d rather you misread it, get sick, come back, and pay for another prescription. It’s a business model.
And the FDA? They’ve known this for 20 years. But they won’t enforce it because Big Pharma lobbies harder than anyone. This isn’t negligence. It’s intentional.
Andrew McAfee
December 6, 2025As someone who grew up in a multilingual household, I can tell you-translation isn’t enough. You need cultural context. 'Take with food' means something different if your family eats rice at 7am vs. toast at 8am.
Pharmacies need to hire bilingual staff who understand local eating habits, not just translate words. A label in Spanish won’t help if the patient thinks 'food' means meat, not chapati.
Andrew Camacho
December 8, 2025Oh wow, another 'poor people are dumb' article. Let me guess-next you’ll say we should teach them to read better? Newsflash: the problem isn’t the patient. It’s the system that treats human beings like machines.
And don’t give me that 'ask your pharmacist' nonsense. They’re rushed, overworked, and paid by the pill, not the patient. You think they have time to explain 'q.i.d.' to 20 people an hour? Wake up.
This isn’t education. It’s exploitation dressed up as concern.
Timothy Sadleir
December 8, 2025Did you know that the FDA’s own 2018 audit found that 63% of prescription labels violated their own plain language guidelines? And yet, no penalties. No fines. No consequences. This is systemic corruption. The same corporations that profit from your illness are the ones writing the labels.
And now they want you to scan a QR code? That’s not innovation. That’s a distraction tactic. They know you won’t trust the label, so they give you a digital illusion of safety. It’s psychological manipulation.
And don’t get me started on Amazon Pharmacy’s voice feature. It’s a Trojan horse for data harvesting. Your voice, your habits, your health-sold to advertisers. You’re not getting help. You’re being monetized.
Shirou Spade
December 9, 2025It’s funny how we blame the patient for not understanding Latin terms that haven’t been used in clinical practice since the 1800s. We still use 'q.d.' and 'b.i.d.' because tradition > clarity.
But here’s the deeper truth: language is power. If you control the words, you control the outcome. The pharmaceutical industry doesn’t want you to understand the label. They want you to take it, not question it.
So when you misread it, it’s not your fault. It’s the design of silence.
Andrew Camacho
December 10, 2025Wait, you’re telling me someone actually read the label? That’s the real tragedy.
Most people just glance at the pill color and hope for the best. If it’s blue, it’s the same as last time. If it’s white, it’s probably the same. That’s how it works. Labels are decoration. Not instructions.
So yeah, make them clearer. But don’t pretend people are reading them. They’re not. They’re trusting. And that’s the real problem.