Antidepressant Withdrawal: What Happens When You Stop Too Soon
When you stop taking antidepressants, medications prescribed to treat depression, anxiety, and other mood disorders by balancing brain chemicals like serotonin and norepinephrine. Also known as antidepressant discontinuation syndrome, it’s not a relapse—it’s your body reacting to the sudden absence of a drug it’s come to rely on. This isn’t rare. Up to 1 in 3 people who quit antidepressants abruptly experience withdrawal, even if they’ve only been on them for a few weeks. It’s not weakness. It’s biology.
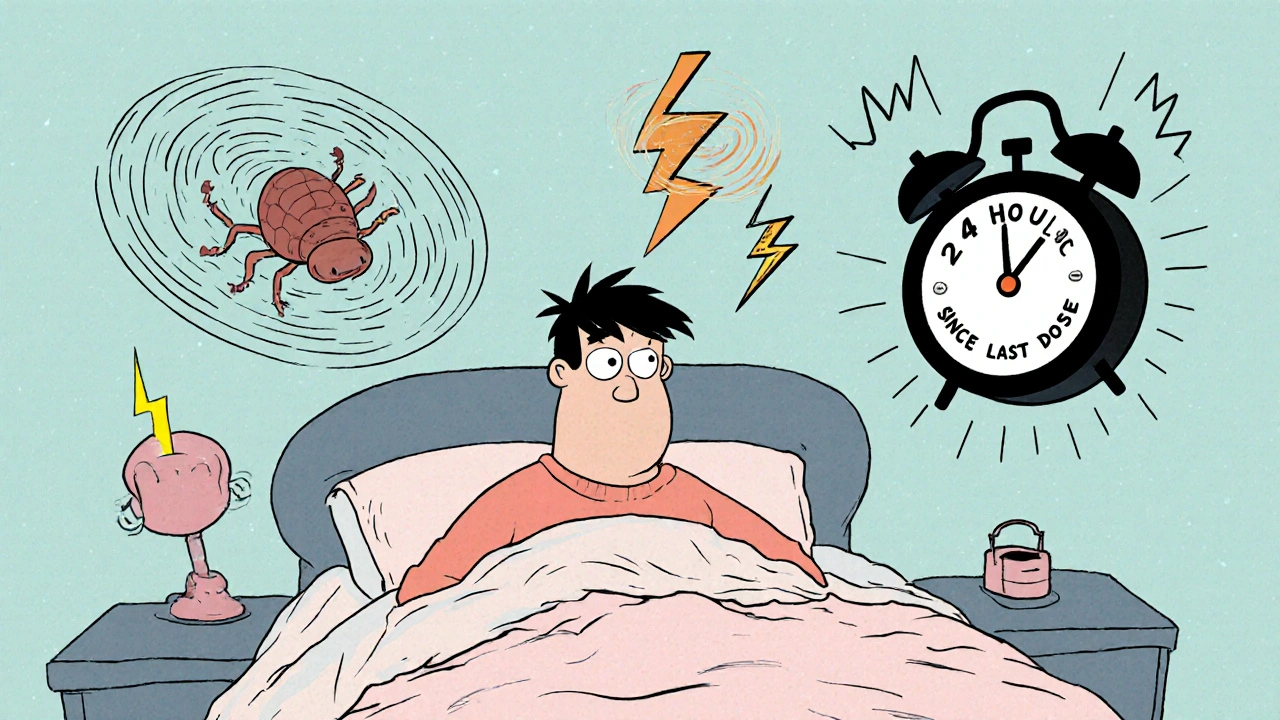
What you feel during antidepressant withdrawal, a set of physical and mental symptoms that occur after stopping or reducing antidepressant dosage can be confusing. Dizziness, electric shock sensations in your head (called brain zaps), nausea, insomnia, anxiety, and mood swings are common. Some people feel like they’re coming down with the flu. Others say their emotions feel raw, like nerves are exposed. These aren’t signs you’re getting sicker—they’re signs your brain is rewiring itself. The same drugs that help stabilize your mood also alter how your neurons communicate. When you remove them too fast, your brain doesn’t have time to adjust.
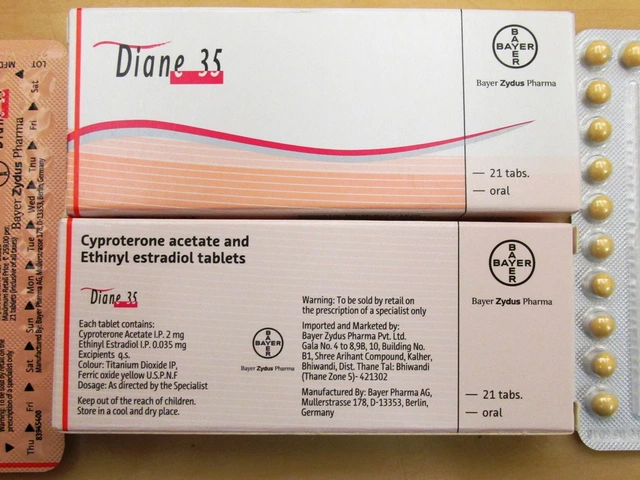
Not all antidepressants are the same when it comes to withdrawal. SSRIs, a class of antidepressants that increase serotonin levels in the brain, commonly prescribed for depression and anxiety like sertraline or fluoxetine have different withdrawal profiles. Short-acting ones like paroxetine or venlafaxine tend to cause stronger symptoms because they leave your system faster. Longer-acting ones like fluoxetine (Prozac) are gentler on the way out. But even Prozac can trigger withdrawal if you’ve been on it long-term. The key isn’t just the drug—it’s how you stop. Tapering slowly, under medical supervision, cuts your risk of severe symptoms by half or more.
And here’s something most people don’t know: withdrawal can start days or even weeks after your last pill. You might feel fine for a while, then suddenly crash. That’s why stopping cold turkey—even if you think you’re ready—is risky. Some people try to quit on their own because they’re embarrassed, afraid of side effects, or think they don’t need help anymore. But skipping the taper can turn a manageable process into a weeks-long struggle. You don’t have to stay on antidepressants forever, but quitting safely takes planning.
What you’ll find below are real, practical stories and science-backed guides on what happens when you stop antidepressants, how to recognize the warning signs, why some people suffer more than others, and what alternatives exist if you want to get off safely. You’ll see how caffeine, alcohol, and even other meds can make withdrawal worse. You’ll learn why switching brands of lithium or generic drugs can affect your mood stability. And you’ll find out how to talk to your doctor about tapering without being dismissed. This isn’t about fear. It’s about control. You deserve to end your treatment on your terms—with your health intact.