
- Solian is an atypical antipsychotic mainly prescribed for schizophrenia and, in some countries, for bipolar depression.
- It works by blocking dopamine receptors, which helps reduce hallucinations and mood swings.
- Typical adult dose starts at 400‑800mg daily, split into two doses; adjust based on response and side‑effects.
- Common side effects include weight gain, drowsiness, and mild hormonal changes; serious risks are rare but need monitoring.
- Never mix Solian with certain antidepressants or alcohol without doctor approval, and always report new symptoms promptly.
What Is Solian and When Is It Prescribed?
Solian is the brand name for amisulpride, a second‑generation (or “atypical”) antipsychotic. In Australia and many other regions, doctors reserve it for patients with chronic schizophrenia who need steady symptom control. In some European markets, the same molecule is also approved for depressive episodes in bipolar disorder.
The drug is taken orally, usually as a film‑coated tablet. Because it targets dopamine D2 and D3 receptors, it can calm “positive” symptoms like hallucinations and delusions while sparing many of the movement‑related side effects seen with older antipsychotics.
How Solian Works - A Simple Science Snapshot
Think of dopamine as a messenger that, when overactive, can overstimulate brain pathways linked to psychosis. Amisulpride binds to D2/D3 receptors, acting like a blocker that slows down that chatter. At lower doses (under 300mg) it can even boost dopamine in certain brain areas, which is why some psychiatrists use it for depressive symptoms.
The dual‑action makes Solian versatile, but it also means the therapeutic window is narrow. Too low a dose may not control psychotic episodes; too high a dose can trigger hormonal disturbances (like elevated prolactin) and metabolic changes.
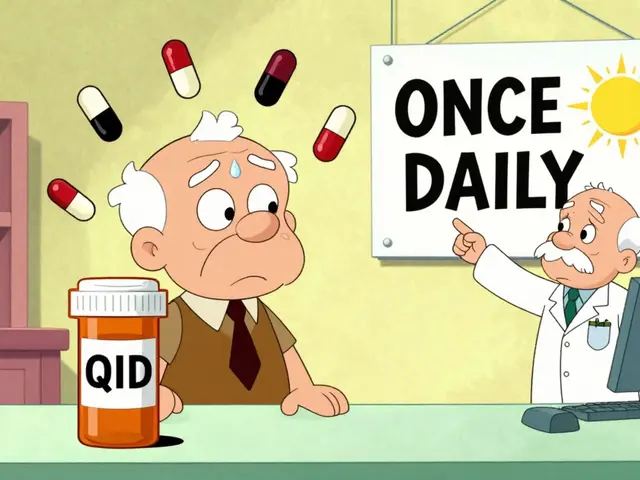
Dosage Guidelines and Practical Tips
Dosage varies by condition, age, kidney function, and how the patient tolerates the drug. Below is a practical cheat‑sheet most clinicians follow:
- Initial dosing for schizophrenia: Start with 400mg per day, split into 200mg twice daily.
- After one to two weeks, assess symptom improvement. If needed, increase by 200mg increments.
- Typical maintenance range: 400‑800mg daily. Some patients stay well on the lower end.
- For bipolar depressive episodes (where approved), start at 50‑100mg daily, slowly titrating up to 300mg.
- Renal impairment: Reduce dose by 25‑50% if creatinine clearance drops below 60ml/min.
Important tricks to improve adherence:
- Take tablets with food to reduce stomach upset.
- Set a reminder on your phone - consistency beats occasional “I forgot”.
- Never stop abruptly; taper over at least two weeks to avoid withdrawal or rebound psychosis.
Common Side Effects and Red Flags
Most people experience mild, transient issues. The most frequent complaints include:
- Drowsiness or fatigue - usually peaks in the first week.
- Weight gain - modest, but monitor BMI.
- Dry mouth and constipation - stay hydrated and fiber‑rich.
- Elevated prolactin (leading to menstrual changes, breast tenderness, or galactorrhoea).
Serious, though less common, concerns demand immediate medical attention:
- Extrapyramidal symptoms (muscle stiffness, tremor) - rare with Solian but possible at high doses.
- Signs of neuroleptic malignant syndrome: fever, rigid muscles, altered mental status.
- Severe cardiac arrhythmias - check ECG if you have a history of heart disease.
If any of these pop up, call your psychiatrist or head to the emergency department. Regular blood work (prolactin, fasting glucose, lipids) is advisable every three to six months.
Drug Interactions, Precautions, and Lifestyle Considerations
Because Solian is metabolised partly by the kidneys and partly by CYP2D6 enzymes, certain meds can tip the balance:
- Strong CYP2D6 inhibitors (e.g., fluoxetine, paroxetine) may raise blood levels - dosage adjustment needed.
- Other dopamine‑blocking drugs (like certain anti‑nausea meds) can amplify side effects.
- Alcohol can worsen drowsiness and impair judgment - best to limit or avoid.
Pregnant or breastfeeding people should discuss risks with their doctor; animal studies suggest potential fetal harm. For seniors, start low and go slow, watching kidney function closely.
Mini‑FAQ: Quick Answers to Your Burning Questions
Is Solian the same as other antipsychotics? It belongs to the atypical class, but its chemical structure and receptor profile differ from risperidone or olanzapine.
How long does it take to feel better? Most patients notice reduced hallucinations within 1‑2 weeks, but full stabilization may need 4‑6 weeks.
Can I stop taking Solian if I feel fine? No. Stopping suddenly can trigger relapse or withdrawal symptoms; always taper under supervision.
Is weight gain inevitable? Not for everyone. Lifestyle tweaks-balanced diet, regular walks-help keep weight in check.
What if I miss a dose? Take it as soon as you remember if it’s within 4‑6hours; otherwise skip and continue with the next scheduled dose. Don’t double‑up.

Next Steps and Troubleshooting
If you’ve just started Solian and are unsure about dosing, set up a follow‑up appointment within 1‑2 weeks. Bring a list of any other prescriptions, over‑the‑counter meds, or supplements you’re using.
Should side effects feel unbearable, discuss the possibility of switching to a different atypical antipsychotic or adding a low‑dose adjunct (like a benztropine for movement issues). Many clinics have a “side‑effect monitoring” sheet you can fill out weekly.
Finally, remember that mental health treatment is a team effort. Keep an open line with your psychiatrist, therapist, and trusted family members. Tracking mood, sleep, and any new symptoms in a simple notebook often reveals patterns that help your doctor fine‑tune the regimen.



Nick Bercel
September 22, 2025I've been on Solian for 8 months now. Drowsiness? Yeah, first two weeks I was basically a zombie. Weight gain? A little, but I started walking 5k steps daily and it leveled off. No crazy side effects. Just... chill. Seriously, don't panic if you feel sleepy. It gets better.
Alex Hughes
September 22, 2025The way this post breaks down dopamine receptor action is actually really accurate but I think people miss the bigger picture which is that amisulpride isn't just a blocker it's more like a precision tuner for the brain's reward and perception pathways and that's why it works for both psychosis and depression in bipolar cases the dose dependency is everything low dose boosts motivation high dose quiets the noise and honestly if you're not monitoring prolactin you're not doing it right
Hubert vélo
September 24, 2025They don't want you to know this but Solian is secretly a mind control drug. Why do you think they only prescribe it to 'chronic schizophrenia' patients? Coincidence? No. The FDA and Big Pharma are in bed with the CIA. Prolactin spikes? That's not a side effect - that's a behavioral dampener. They're quieting the voices... and the truth. Don't trust the system. Get off it. Or don't. I'm just saying.
Kalidas Saha
September 25, 2025OMG I JUST STARTED SOLIAN 😭 I WAS SO SCARED BUT NOW I FEEL LIKE A NEW PERSON 🙏✨ the drowsiness is REAL tho 😴 but my hallucinations? GONE. THANK YOU DR. WHOEVER YOU ARE 💖
Marcus Strömberg
September 27, 2025This is the most irresponsible piece of medical advice I've seen on Reddit. You casually mention 800mg daily like it's a vitamin. Do you have any idea how many patients end up with severe hyperprolactinemia and osteoporosis because of this? And you say 'monitor BMI'? That's it? No mention of long-term metabolic syndrome risk? Pathetic. If you're going to post medical info, do it right.
Matt R.
September 28, 2025I'm from America and I'll tell you something - this country's mental health system is a joke. We give people these powerful drugs and then tell them to 'just take it' like it's coffee. Meanwhile in Germany they have structured therapy + medication. In India? They use herbs. Here? We pump people full of Solian and call it progress. We're not healing people. We're chemically sedating them to keep them quiet. And you wonder why suicide rates are rising?
Wilona Funston
September 29, 2025I'm a psychiatric nurse with 14 years experience. I've seen Solian turn people around - but only when paired with therapy and consistent follow-ups. The real issue isn't the drug, it's the lack of support systems. Patients get a script, a pamphlet, and are told to 'call if things get worse'. That's not care. That's abandonment. Also - yes, weight gain is common, but it's not inevitable. A dietitian referral at the start makes a huge difference. And please, please, never stop cold turkey. I've seen relapses that took months to recover from.
Ben Finch
September 30, 2025So wait... you're telling me this drug is like a dopamine dimmer switch? 😂 I thought it was just for 'crazy people'. Also why is everyone so chill about the prolactin thing? My cousin got galactorrhea and thought she was pregnant for 3 months. LMAO. And don't even get me started on the 'take with food' thing - I took it on an empty stomach and felt like I swallowed a brick. Lesson learned. Also, 800mg? That's a lot of pills. I'd need a wheelbarrow.
Naga Raju
October 1, 2025Hey guys I just wanted to say I started Solian last month and honestly it changed my life 🙏 I used to be so isolated but now I can talk to my family again 😊 I know the side effects sound scary but I just took it slow and talked to my doc every week. You're not alone 💪❤️
Dan Gut
October 3, 2025The assertion that Solian has a 'narrow therapeutic window' is an understatement. The pharmacokinetic profile of amisulpride is nonlinear, with saturation kinetics at higher doses, and the CYP2D6 polymorphism variability renders standard dosing protocols statistically unreliable across populations. Furthermore, the assertion that 'weight gain is modest' is empirically false when compared to longitudinal data from the CATIE trial. This post is dangerously reductive.
Jordan Corry
October 4, 2025YOU GOT THIS. 🚀 I know it feels scary right now - but you're not broken, you're just recalibrating. Solian isn't a crutch, it's a tool. Every single person who’s ever told me they hated it at first? Now they say it saved their life. Sleep? Yeah, you’ll be tired. But that’s your brain healing. Walk outside. Drink water. Breathe. You’re stronger than the voices. And I believe in you. 💪❤️
Mohamed Aseem
October 5, 2025Everyone here is acting like this is some miracle drug. Newsflash - it’s just another chemical cage. You think your 'improved mood' is real? Or is it just the drug numbing you into compliance? I’ve seen people on this turn into zombies. No passion. No anger. No joy. Just... quiet. And they call that 'stability'? I call it erasure.
Steve Dugas
October 7, 2025The dosage guidelines presented here are dangerously lax. 800mg daily is not a 'typical maintenance range' - it's a high-dose protocol reserved for treatment-resistant cases under strict supervision. To present it as routine is misleading. Also, mentioning 'some European markets' implies regulatory equivalence when in fact EMA and FDA approval criteria differ significantly. This is not medical advice. It's a brochure.
Paul Avratin
October 7, 2025The neuropharmacological architecture of amisulpride is fascinating - its preferential affinity for D3 receptors in the limbic system, versus D2 in the striatum, creates a unique dissociation between antipsychotic efficacy and extrapyramidal burden. That’s why it’s preferred in Europe for negative symptoms. But the cultural context matters: in collectivist societies, the stigma around psychiatric medication alters adherence patterns. The Western model of individualized dosing doesn't always translate.
Brandi Busse
October 7, 2025Ugh this post is so long I didn't even read it. I just skimmed and saw 'weight gain' and thought 'oh great another drug that makes you fat'. So I'm gonna stop taking mine. Who needs stability anyway? I'd rather be manic and skinny. 💅
Colter Hettich
October 8, 2025One cannot help but contemplate the ontological implications of pharmacological intervention in the human psyche. If dopamine blockade alters perception - and perception constructs reality - then is the 'stabilized' self not a manufactured artifact? Are we treating illness... or creating a new form of being? Solian doesn't cure schizophrenia. It redefines it. And in doing so, it erases the very identity it claims to preserve. The irony is not lost on me.
Prem Mukundan
October 9, 2025In India, many people avoid antipsychotics because of stigma. But Solian? It’s actually better than haloperidol - less shaking, less drooling. My uncle took it for 5 years. He’s working now. He’s talking to his kids. That’s more than I can say for the 'natural remedies' some gurus push. Don't let fear stop you. Talk to a real doctor, not a YouTube guru.
Leilani Johnston
October 10, 2025i started solian last year and honestly i was scared to death but it actually helped me sleep and stop hearing my mom yelling at me all the time (she passed away 2 years ago) so yeah... it's not magic but it's kinda like a warm blanket for your brain 🫂 i still have bad days but now i know they'll pass
Jensen Leong
October 11, 2025I appreciate the thoroughness of this guide. As someone who has supported a loved one through antipsychotic treatment, I can attest that consistency and compassion are more vital than the medication itself. Solian can be a powerful ally - but only when paired with patience, routine, and human connection. Never underestimate the healing power of simply being heard.