
Fournier's Gangrene Risk Checker
This tool helps you recognize emergency signs of Fournier's gangrene linked to SGLT-2 inhibitor diabetes medications. Do NOT use this to diagnose or treat. If you have severe symptoms, go to the ER immediately.
Most people taking SGLT-2 inhibitors for type 2 diabetes never hear about Fournier’s gangrene-until it’s too late. This isn’t a distant medical oddity. It’s a real, fast-moving infection that can turn a routine prescription into a life-or-death situation. And it’s happening more often than you think.
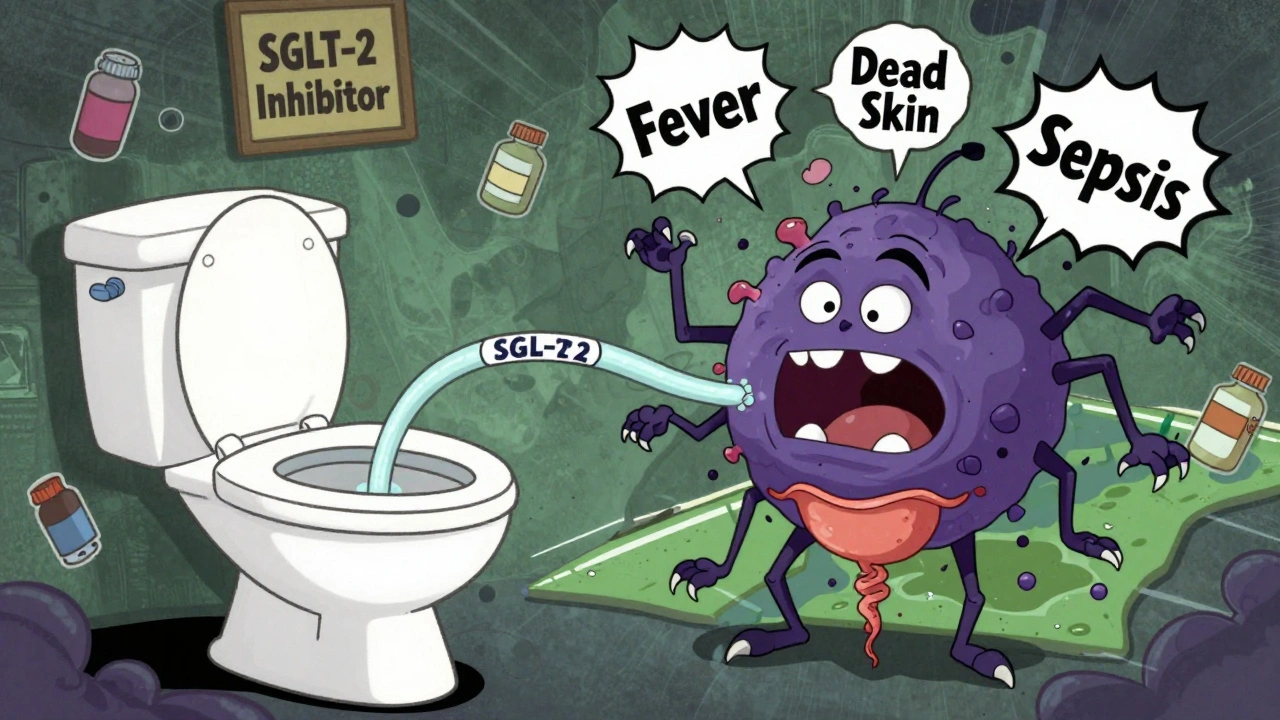
What Is Fournier’s Gangrene?
Fournier’s gangrene is a rare but deadly bacterial infection that eats away at skin and tissue around the genitals and anus. It doesn’t wait for permission. It spreads fast-sometimes in hours. What starts as mild discomfort can quickly become unbearable pain, swelling, and foul-smelling discharge. Without emergency treatment, it can lead to sepsis, organ failure, or death.
For decades, this condition was seen mostly in older men with diabetes, obesity, or weakened immune systems. But since 2013, something new has emerged. Cases are popping up in women, younger adults, and people who were otherwise healthy-people taking medications like Jardiance, Farxiga, Invokana, and Steglatro.
The Link to SGLT-2 Inhibitors
SGLT-2 inhibitors work by making your kidneys flush out extra sugar through urine. That sounds good-it lowers blood sugar. But that sugar doesn’t just disappear. It stays in your urinary tract, creating a sweet breeding ground for bacteria and fungi.
This is why genital yeast infections and urinary tract infections are common side effects of these drugs. For most people, it’s a nuisance. For a small number, it becomes a gateway to something far worse. The bacteria don’t stop at the surface. They dig deeper, infecting the fascia-the connective tissue under the skin-and from there, they start destroying everything in their path.
The U.S. FDA issued a boxed warning in August 2018 after 12 cases were reported between 2013 and 2018. By 2022, New Zealand’s Medsafe and the UK’s MHRA had also updated their safety alerts. The numbers are small-about one case per 10,000 men treated-but when it hits, it hits hard. And it’s not just men anymore. About one-third of reported cases are in women, which flips the old medical assumption on its head.
Emergency Signs You Must Recognize
If you’re taking one of these medications, you need to know the warning signs. Don’t wait. Don’t assume it’s a minor infection. If you notice any of these, go to the ER immediately:
- Severe pain in the genital or anal area-pain that feels worse than it looks
- Redness, swelling, or warmth around the genitals, scrotum, or anus
- Fever or chills that come on suddenly
- Foul-smelling discharge from the genital or anal area
- Dark or dead-looking skin in the area, sometimes with blisters or bubbles
- General feeling of being very sick-malaise, dizziness, confusion
One case reported in a medical journal described a 71-year-old woman on dapagliflozin who developed a large abscess and foul-smelling discharge. She didn’t have a history of severe diabetes complications. She was just taking her pill every morning. Within days, she was in intensive care.
Don’t dismiss these symptoms as a yeast infection or a pimple. Fournier’s gangrene doesn’t look like a rash. It looks like tissue is dying. And time is everything.
What Happens If It’s Not Treated Fast?
There’s no magic pill for Fournier’s gangrene. Treatment is brutal and urgent:
- Stop the medication immediately-your doctor will switch you to a different diabetes drug
- High-dose IV antibiotics to fight the infection
- Surgery to remove dead tissue-often multiple procedures
- Intensive care-most patients need it
In one study of 19 patients with SGLT-2 inhibitor-linked Fournier’s gangrene, 78.9% ended up in intensive care. 63.2% needed more than one surgery. And 15.8% died-even with full treatment.
That’s not a risk you can afford to gamble with.
Who’s at Higher Risk?
Not everyone taking SGLT-2 inhibitors will get this. But some people are more vulnerable:
- People with type 2 diabetes, especially if blood sugar is poorly controlled
- Those with obesity (BMI over 30)
- People over 65
- Those with a history of genital infections
- Anyone with weakened immunity from other conditions or medications
- Women under 50-this group wasn’t considered at risk before, but now we know better
Even if you don’t fit the “classic” profile, you’re not immune. The FDA and other agencies have seen cases in people with no obvious risk factors other than the drug itself.

Should You Stop Taking Your Medication?
No. Not without talking to your doctor.
SGLT-2 inhibitors are powerful drugs. They don’t just lower blood sugar-they reduce the risk of heart failure, kidney disease, and death from cardiovascular causes. For many people, the benefits far outweigh the risk of this rare complication.
But that doesn’t mean you should ignore the danger. If you’re on one of these medications, here’s what to do:
- Know the signs. Memorize them.
- Talk to your doctor about your personal risk.
- Ask if you’re a good candidate for this drug, especially if you’ve had recurrent yeast infections.
- Don’t wait for symptoms to get worse. If something feels off, go to the hospital.
Doctors are now required to warn patients about this risk when prescribing these drugs. If your doctor hasn’t mentioned it, ask. It’s your right to know.
What Are the Alternatives?
If you’re worried, there are other diabetes medications that don’t carry this risk:
- Metformin-the first-line treatment for type 2 diabetes
- GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or liraglutide (Victoza)
- DPP-4 inhibitors like sitagliptin (Januvia)
- Insulin, if needed
None of these have been linked to Fournier’s gangrene. Your doctor can help you switch safely, especially if you’re already experiencing frequent genital infections or have other risk factors.
What to Do Right Now
If you’re taking Jardiance, Farxiga, Invokana, or Steglatro:
- Check your genital area daily-look for redness, swelling, or sores
- Don’t ignore itching, burning, or unusual discharge
- Keep your blood sugar under control-high glucose makes infections worse
- Stay hydrated and practice good hygiene
- If you notice any warning signs, go to the emergency room immediately
There’s no time to wait. Fournier’s gangrene doesn’t wait. And neither should you.
Can women get Fournier’s gangrene from diabetes medications?
Yes. While Fournier’s gangrene was historically thought to affect mostly men, cases linked to SGLT-2 inhibitors like Jardiance and Farxiga have occurred in women at nearly one-third the rate of men. This is a recent shift recognized by global health agencies, and women under 50 are now being identified as a vulnerable group.
How soon after starting the medication can Fournier’s gangrene develop?
Cases have appeared within weeks to several months after starting the drug. The FDA found that most patients developed symptoms within 3 to 6 months of beginning treatment. But there have been reports as early as 2 weeks after starting the medication.
Is Fournier’s gangrene curable?
It’s treatable-but only if caught early. Treatment requires emergency surgery to remove dead tissue, strong IV antibiotics, and intensive care. Even with full treatment, 15% of patients die. Delaying care dramatically increases the risk of death or permanent damage.
Do I need to stop my diabetes medication if I get a yeast infection?
Not necessarily. Mild yeast infections are common with SGLT-2 inhibitors and can be treated with antifungal creams or pills. But if the infection doesn’t clear up, keeps coming back, or is accompanied by pain, swelling, or fever, stop the medication and see your doctor immediately. Recurrent infections could be a warning sign.
Are all SGLT-2 inhibitors equally risky?
All SGLT-2 inhibitors-canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin-carry the same risk. The mechanism that causes increased sugar in urine applies to all of them. Regulatory agencies have issued warnings for all drugs in this class, not just one brand.
Can I switch to a different diabetes drug safely?
Yes. Many people switch to metformin, GLP-1 agonists like Ozempic, or DPP-4 inhibitors without issue. Your doctor can help you transition safely while keeping your blood sugar stable. Never stop your medication abruptly without medical guidance, but do discuss alternatives if you’re concerned about this risk.
If you’re taking an SGLT-2 inhibitor, your health is not just about your A1C. It’s about knowing what your body is telling you-and acting before it’s too late. This isn’t fearmongering. It’s medicine. And it’s urgent.



Sean McCarthy
December 2, 2025My uncle got this after starting Jardiance. Went from "just a little itch" to ICU in 36 hours. No joke. They had to amputate half his pelvis. Don't ignore redness. Don't wait. Go to the ER.
ANN JACOBS
December 3, 2025It is of paramount importance that individuals currently prescribed SGLT-2 inhibitors, particularly those with comorbid conditions such as obesity or immunocompromised states, remain vigilant regarding any novel or escalating genital or perineal symptoms. The pathophysiological mechanism-namely, glycosuria-induced microbial proliferation-has been robustly documented in peer-reviewed literature since 2018, and the clinical imperative for early surgical intervention cannot be overstated. Delayed diagnosis correlates directly with mortality rates exceeding 15 percent, even with aggressive multimodal therapy.
Nnaemeka Kingsley
December 4, 2025bro i just started farxiga last month and had yeast infection 2 times already. i was gonna ignore it but now im scared. should i stop or just wait? i dont wanna die for a pill
Linda Migdal
December 5, 2025Of course the FDA only acts after Americans start dying. Meanwhile, Europe and Canada warned us two years earlier. This is what happens when you let corporate lobbyists write your drug policy. We need real oversight, not PR statements.
Tommy Walton
December 6, 2025Life is just a series of biochemical trade-offs. You want longevity? You pay with risk. The real question isn’t whether this drug is dangerous-it’s whether you’re willing to live with the consequences of inaction. 🧠💀
James Steele
December 8, 2025The elegance of SGLT-2 inhibition lies in its elegant osmotic diuresis-yet the unintended consequence is a metabolic Eden for opportunistic pathogens. The fascial necrosis isn't merely bacterial-it's a systemic betrayal of homeostasis. This isn't a side effect. It's a cascade failure.
Louise Girvan
December 9, 2025Big Pharma knew. They buried the data. Your doctor doesn't care. They get paid to prescribe. You're a lab rat. Wake up.
soorya Raju
December 10, 2025Wait wait wait. This is all a CIA psyop to make people stop taking diabetes meds so they can control the population with insulin. The real killer is glyphosate in your bread. I read it on a forum in Kerala. Trust me.
Grant Hurley
December 11, 2025just checked my groin real quick after reading this… no redness, no swelling, no weird smell. phew. but im gonna keep checking daily now. better safe than sorry. thanks for the heads up.
Lucinda Bresnehan
December 12, 2025i'm a nurse in a rural ER. we had a 42-year-old woman come in last month with this. she was on dapagliflozin, no other risk factors. she thought it was just a bad yeast infection. by the time she came in, the infection had eaten through her perineum. we saved her life, but she'll never walk the same again. please, if you're on one of these drugs, listen. it's not fear-it's awareness.
Shannon Gabrielle
December 14, 2025Oh wow, a drug that makes you pee sugar? Genius. Next they'll make us drink bleach to lose weight. Let me guess-this was approved because it lowered A1C by 0.3%? Congrats, you just traded a man’s genitals for a lab result.
Kshitij Shah
December 14, 2025in india we don't even have access to these drugs. but my cousin in texas got it. she's lucky she's alive. the hospital bill was 2 million rupees. you think your insurance covers this? lol.
Dennis Jesuyon Balogun
December 15, 2025Human biology was never meant to be manipulated by pharmacological precision. We are not machines. When we override natural regulatory systems-like renal glucose excretion-we invite chaos. This is not a side effect. It is the inevitable consequence of reducing life to a metabolic equation. The body remembers. And when it retaliates, it does not ask permission.
Lauryn Smith
December 16, 2025i’m so glad i read this. i’ve been on Invokana for a year and had two yeast infections. i thought it was just me. i’m calling my doctor tomorrow to switch. thank you for sharing this.
elizabeth muzichuk
December 18, 2025How dare you normalize this? People are dying because we let corporations sell poison as medicine. You should be ashamed. This is why America is collapsing.