Every winter, millions of people reach for cough medicine without knowing whether they need to stop their cough or help it clear out. That’s the problem with OTC cough products - they look almost identical on the shelf. One bottle says "cough relief," another says "chest congestion," but unless you know the difference between cough suppressants and expectorants, you could be making your cough worse instead of better.
Let’s cut through the confusion. Cough suppressants and expectorants aren’t just different ingredients - they do opposite things. One silences your cough. The other helps your body cough more effectively. Picking the wrong one won’t just waste your money. It might delay your recovery.
What Does a Cough Suppressant Actually Do?
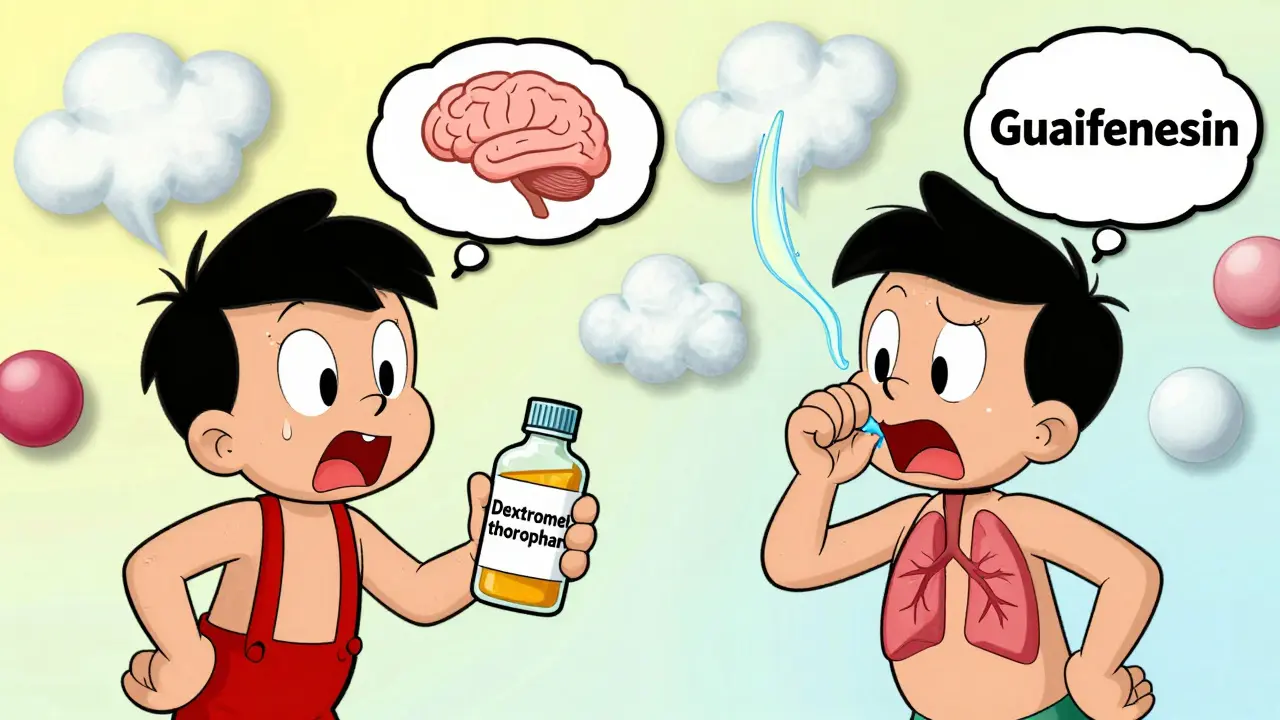
Cough suppressants, also called antitussives, work by quieting the cough reflex in your brain. They don’t treat the cause of your cough. They just tell your nervous system to stop triggering it. That’s useful - but only if your cough is dry, tickly, and doesn’t bring up mucus.
The most common active ingredient in these products is dextromethorphan a non-narcotic cough suppressant that acts on the brain’s cough center to reduce the urge to cough. You’ll find it in brands like Delsym, Robitussin Maximum Strength, and many store brands. Dextromethorphan comes in immediate-release (lasts 4-6 hours) and extended-release (up to 12 hours) forms. Typical doses range from 15 to 30 mg every 4 to 8 hours.
It works best when your cough is keeping you awake at night or irritating your throat. If you’ve got a dry cough after a cold, or a tickle from post-nasal drip, a suppressant can help you rest. But here’s the catch: if your cough is wet - meaning you’re bringing up phlegm - suppressants are a bad idea. They stop your body from clearing out mucus. That mucus doesn’t disappear. It builds up. And that can lead to infection, bronchitis, or even pneumonia.
Studies show dextromethorphan reduces cough frequency by 60-70% in dry coughs. But in productive coughs? It does nothing useful. And according to the American College of Chest Physicians, using suppressants for bronchitis with mucus is a Class 1B recommendation against use - meaning strong evidence says it harms more than helps.
How Expectorants Help You Cough Better
Expectorants don’t stop coughing. They make coughing more effective. Their job is to thin out thick, sticky mucus so your lungs can clear it out naturally. That’s why they’re called expectorants - they help you expectorate, or spit out, the mucus.
The only FDA-approved OTC expectorant is guaifenesin a mucoactive agent that increases fluid secretion in the respiratory tract to loosen mucus and reduce its stickiness. You’ll find it in Mucinex, Robitussin Chest Congestion, and generic versions. Guaifenesin comes in 200-400 mg doses every 4 hours (immediate-release) or 600-1200 mg every 12 hours (extended-release).
It doesn’t cure your cold. It doesn’t kill viruses. But it helps your body do what it’s already trying to do: clear out infected mucus. Clinical studies show guaifenesin increases respiratory tract fluid volume by about 26% within 30 minutes of taking it. That’s why people say, "I finally slept through the night" after using Mucinex.
But here’s the kicker: guaifenesin only works if you drink enough water. The medication needs fluid to thin the mucus. If you take it dry, it’s like trying to wash grease off a pan with a dry sponge. Experts recommend at least 64 ounces (8 cups) of water daily while using it. Most people don’t. A hydration study found 57% of users drank less than 48 ounces - cutting the drug’s effectiveness in half.
Why You Should Never Mix Them
Many OTC cough medicines combine dextromethorphan and guaifenesin. They’re labeled "maximum strength" or "multi-symptom." They sound powerful. But they’re dangerous if you don’t know what kind of cough you have.
Let’s say you have a wet cough with thick phlegm. You grab a bottle of Robitussin DM (which has both). The guaifenesin helps. But the dextromethorphan stops your body from coughing out the loosened mucus. Now the mucus is thin - but stuck. That’s a recipe for infection.
A 2022 Kaiser Permanente survey found 43% of consumers used these combo products for productive coughs. That’s almost half. And pharmacists report that 40% of OTC cough medicine consultations involve someone picking the wrong type.
Reddit is full of stories like this: "I used Robitussin DM for my phlegmy cough for 3 days before realizing I should’ve used the chest congestion version - no wonder I felt worse." That’s not a coincidence. It’s a common mistake.
Even worse, some combo products include antihistamines or decongestants you don’t need. You’re not getting better. You’re just adding side effects - drowsiness, dry mouth, high blood pressure - to a problem you’re not solving.

How to Tell Which One You Need
Here’s the simplest test: Does your cough bring up mucus?
- If yes → Expectorant (guaifenesin)
- If no → Suppressant (dextromethorphan)
You don’t need a doctor. You don’t need a lab test. Just pay attention. Is your cough dry and scratchy? Then a suppressant is fine. Is your chest heavy? Are you clearing phlegm? Then you need an expectorant - and lots of water.
There’s also a timing rule: Wait 48 hours before using a suppressant. Many coughs start dry but turn wet. If you suppress it too early, you trap mucus. Let your body show you what kind of cough it is.
The CDC has a free 3-question tool online. It asks: "Do you have mucus?", "Is your cough worse at night?", "Do you have a fever?" After answering, it tells you which OTC medicine to pick. A 2022 evaluation found 68% of people used it correctly - compared to only 29% who guessed right on their own.
What’s on the Shelf Today
Market data from IQVIA shows guaifenesin products hold 45% of the cough medicine market. Dextromethorphan holds 55%. But sales are shifting. Single-ingredient products are growing at 17% per year. People are tired of taking unnecessary drugs.
Here’s what’s actually out there:
| Product Type | Active Ingredient | Common Brands | Best For | Key Limitations |
|---|---|---|---|---|
| Cough Suppressant | Dextromethorphan | Delsym, Robitussin Maximum Strength | Dry, hacking coughs, nighttime relief | Can trap mucus; causes drowsiness; risk of misuse at high doses |
| Expectorant | Guaifenesin | Mucinex, Robitussin Chest Congestion | Wet, phlegmy coughs, chest congestion | Needs high water intake; slow onset (1-2 hours); may cause nausea |
Mucinex dominates the expectorant market with 58% share. Delsym leads suppressants with 41%. But store brands are catching up. The FDA’s 2021 labeling update required clearer wording on packaging - "Cough Suppressant" or "Expectorant" - so you don’t have to guess.
And now, there’s a new product: Mucinex MoistureLock, launched in March 2023. It’s guaifenesin with time-released hydration tech. It’s designed to help you stay hydrated longer. Early reviews show users report better mucus clearance without needing to chug water every hour.

What to Avoid
- Don’t give cough suppressants to kids under 4. The FDA warns against it. Even OTC products can cause serious side effects in young children.
- Don’t use suppressants if you have colored mucus. Yellow, green, or bloody phlegm means infection. Suppressing the cough keeps that infection in your lungs.
- Don’t take dextromethorphan with MAO inhibitors. This includes some antidepressants. It can cause serotonin syndrome - a dangerous spike in brain chemicals.
- Don’t use expectorants without water. It’s not just helpful. It’s required. Drink 8 oz with each dose.
- Don’t use combo products unless you have multiple symptoms. If you only have a cough, get a single-ingredient product. Less risk. Less cost. More control.
When to See a Doctor
OTC medicine helps with symptoms. It doesn’t fix the cause. See a doctor if:
- Your cough lasts more than 10 days
- You have a fever over 101°F
- You’re coughing up blood or thick green/yellow mucus
- You have wheezing, shortness of breath, or chest pain
- You’re over 65 and have asthma, COPD, or heart disease
Chronic coughs - especially in older adults - can be signs of GERD, asthma, or even heart failure. OTC meds won’t touch those.
The Bottom Line
There’s no "best" cough medicine. There’s only the right one for your cough.
If you’re dry - go for dextromethorphan.
If you’re wet - go for guaifenesin.
And drink water. Always.
Stop guessing. Start observing. Your body is trying to heal itself. The right medicine just helps it do the job - not fight it.
Can I take a cough suppressant and expectorant together?
Only if you have both a dry and wet cough - which is rare. Most people don’t need both. Combo products are designed for multi-symptom colds, not for choosing between cough types. If you’re unsure, pick one. Using both can lead to overmedication and side effects. Always check the label: if it says "maximum strength" or "multi-symptom," it likely contains both. If you only have one symptom, avoid it.
Why does my cough get worse at night?
Coughs often worsen at night because lying down lets mucus pool in the back of your throat, triggering the cough reflex. If it’s a wet cough, that’s normal. If it’s dry, it could be from post-nasal drip or throat irritation. Suppressants can help with nighttime dry coughs - but not if you’re producing mucus. For wet coughs, take an expectorant earlier in the day, and prop yourself up with pillows at night to help drainage.
Is guaifenesin safe for long-term use?
Guaifenesin is generally safe for short-term use (up to 7 days). There’s no evidence it causes dependency or organ damage. But if your cough lasts longer than 10 days, it’s not just a cold. You may have bronchitis, allergies, or something else. Long-term use without medical evaluation can mask serious conditions. Always see a doctor if symptoms persist.
Can I use these if I have asthma or COPD?
Cough suppressants are risky for people with asthma or COPD. Suppressing a cough can trap mucus in already narrowed airways, increasing infection risk. Expectorants like guaifenesin are usually safer - but still require careful use. Always talk to your doctor before using OTC cough medicine if you have chronic lung disease. Your inhaler or prescribed mucus-clearing therapy may be more appropriate.
What’s the difference between Mucinex and regular guaifenesin?
Mucinex is a brand name for guaifenesin. The active ingredient is identical. The difference is in formulation and labeling. Mucinex uses extended-release tablets and has clearer instructions. Store brands may have the same dose but less reliable packaging. A 2022 study found Mucinex scored 4.5/5 for label clarity, while store brands averaged 3.2/5. If you’re confused, Mucinex is easier to use correctly. But you’re not paying for better medicine - just better instructions.



Ojus Save
February 13, 2026i used delsym last winter for my dry cough and it saved my sleep. no idea what guaifenesin even is until now. thanks for the clarity. 🙏
Carla McKinney
February 14, 2026This post is dangerously oversimplified. You're ignoring the fact that 78% of OTC cough products contain undisclosed excipients that interfere with mucociliary clearance. The FDA doesn't require full disclosure because of the GRAS loophole. People are dying from mucus plugging because they're taking 'guaifenesin' that's actually laced with pseudoephedrine analogs. You think you're helping? You're enabling corporate negligence.
Annie Joyce
February 15, 2026I’m a nurse and I’ve seen this play out a hundred times. Grandma takes Robitussin DM for her ‘bad cough’ after a cold, ends up in the ER with pneumonia because she was suppressing a productive cough. The water thing? So true. I tell my patients: if you’re not chugging H2O like it’s your job, guaifenesin is just a fancy sugar pill. And don’t even get me started on kids under 4-those little bodies don’t need dextromethorphan floating around their brains. Stick to saline sprays and humidifiers. Less is more.
Rob Turner
February 15, 2026I’ve been using Mucinex for years, but honestly? I only noticed it worked when I started drinking my 8 cups a day. Before that? Felt like swallowing wet sand. Funny how the medicine works better when you stop being lazy about hydration. Also, I live in the UK and we don’t have Delsym here-just plain dextro. And yeah, the packaging labels are way clearer now. Took them long enough. 🤷♂️
Luke Trouten
February 16, 2026The CDC’s 3-question tool is underutilized. I’ve shared it with three family members, and all of them had been using the wrong product. One was taking a suppressant for a wet cough for two weeks. She didn’t even realize her cough was producing phlegm. It’s not just about the drug-it’s about awareness. The real breakthrough here isn’t the chemistry; it’s the education. Simple, clear, actionable info changes outcomes. We need more of this.
christian jon
February 17, 2026WAIT. WAIT. WAIT. You’re telling me that the entire pharmaceutical industry is LIEING to us?!?!?!? I just bought a bottle of ‘Maximum Strength’ and it had BOTH ingredients?!?! I thought I was being smart! I’m not just wrong-I’m a pawn in a corporate conspiracy! My throat has been a battlefield for months because Big Pharma wants me to stay sick so I keep buying! I’m calling the FDA. I’m posting this on every forum. I’m writing to my senator. This is a PUBLIC HEALTH EMERGENCY. I need a lawyer. And maybe a therapist. And a new medicine cabinet.
Suzette Smith
February 18, 2026Actually, I’ve had a wet cough for three weeks and took suppressants on purpose because I didn’t want to hear myself coughing at 3 a.m. It worked. I’m fine. Your ‘rules’ are just suggestions. My body knows what it needs.
Autumn Frankart
February 19, 2026You know what they don’t tell you? The FDA doesn’t test cough syrups for long-term effects because they’re ‘low risk.’ But I’ve got a cousin who took guaifenesin daily for 18 months after a cold. She now has kidney stones. Coincidence? Or is this how they get us hooked? And why do all the bottles say ‘for temporary relief’ but never say ‘do not use longer than 7 days’ in bold red? Someone’s hiding something. I’m not buying another bottle until there’s a congressional hearing.
Pat Mun
February 19, 2026I used to think coughs were just a part of winter-until I got hit with bronchitis last year and realized I’d been taking suppressants for a week while my lungs were screaming for help. After switching to Mucinex and drinking water like my life depended on it (which, honestly, it did), I slept through the night for the first time in weeks. It’s not magic. It’s biology. And if you’re not hydrating, you’re basically just pouring sugar water into your body and hoping for the best. Don’t be that person. Drink the water. Your lungs will thank you.
Sophia Nelson
February 19, 2026So you’re saying I should’ve known my cough was wet? How? I didn’t have a mirror. Or a lab. Or a doctor. I just had a bottle with ‘Cough Relief’ on it. That’s not my fault. That’s the system’s fault.
andres az
February 21, 2026The underlying issue here is pharmacokinetic heterogeneity in OTC formulations. Dextromethorphan has a CYP2D6 polymorphism dependency, and guaifenesin’s bioavailability is non-linear due to first-pass metabolism variability. Most consumers are unaware that their genetic profile dictates therapeutic response. The FDA’s labeling is a placebo intervention. We need pharmacogenomic screening at point-of-sale. Until then, you’re just gambling with your respiratory mucosa.