PPI Selection Calculator for Clopidogrel Therapy
PPI Selection Calculator
Select your PPI and dosage to see the estimated impact on clopidogrel effectiveness.
Results
When you're taking clopidogrel to prevent heart attacks or strokes, you might also need a stomach protector like omeprazole. But here’s the problem: omeprazole can make clopidogrel less effective. This isn’t just a theoretical concern-it’s a real, measurable interaction backed by years of clinical research. If you're on both, you need to understand how and why this happens, and what to do about it.
How Clopidogrel Actually Works
Clopidogrel doesn’t work right away. It’s a prodrug, meaning your body has to turn it into something active before it can block platelets. That activation happens in your liver, and it relies almost entirely on one enzyme: CYP2C19. Without this step, clopidogrel just passes through your system doing nothing. That’s why people with certain genetic variants of CYP2C19-called poor or intermediate metabolizers-often get blood clots even while taking clopidogrel. Their bodies just can’t make enough of the active form.
Why Omeprazole Interferes
Omeprazole is a proton pump inhibitor (PPI) used for acid reflux and ulcers. It’s also metabolized by CYP2C19. But here’s the twist: omeprazole doesn’t just use the enzyme-it blocks it. Think of CYP2C19 as a busy factory line. Clopidogrel needs to go through it to become active. Omeprazole shows up, takes up all the space, and stops clopidogrel from getting processed. The result? Less active clopidogrel in your blood, weaker antiplatelet effect, and higher risk of clots.
Studies show that a standard 20mg dose of omeprazole cuts clopidogrel’s active metabolite by about 32%. At 80mg daily, that drop jumps to 49%. That’s not a small change-it’s enough to affect clinical outcomes, especially in high-risk patients.
Not All PPIs Are the Same
This is where things get practical. Not every stomach medication interferes the same way. The strength of CYP2C19 inhibition varies dramatically between PPIs:
- Omeprazole and esomeprazole (its more potent isomer) are the worst offenders. Both strongly inhibit CYP2C19.
- Lansoprazole has a mild effect-only noticeable at high doses.
- Pantoprazole barely touches CYP2C19. At 40mg daily, it reduces clopidogrel exposure by just 14%.
- Rabeprazole has a moderate effect but doesn’t significantly change overall drug exposure.
- Ilaprazole, a newer option, shows almost no inhibition in recent studies.
So if you need a PPI with clopidogrel, pantoprazole is your safest bet. Rabeprazole is a decent second choice. Omeprazole and esomeprazole? Avoid them entirely.
The Clinical Debate: Does This Actually Cause Heart Attacks?
Here’s the confusion: lab data says one thing. Real-world outcomes say another.
Multiple studies show that omeprazole reduces clopidogrel’s ability to prevent platelet clumping. That’s a clear pharmacodynamic effect. But when you look at actual heart attacks, strokes, or deaths, the picture gets muddy.
The COGENT trial-a large, randomized study of over 3,700 people-found no increase in cardiovascular events when omeprazole was added to clopidogrel. Meanwhile, a massive meta-analysis of 271,000 patients showed a 27% higher risk of bad events with PPI use, with omeprazole being the worst.
Why the contradiction? One major reason: the FAST-MI Registry found no increased risk in real-world patients, but those patients were often monitored closely and had access to better care. The meta-analysis included higher-risk populations with less control.
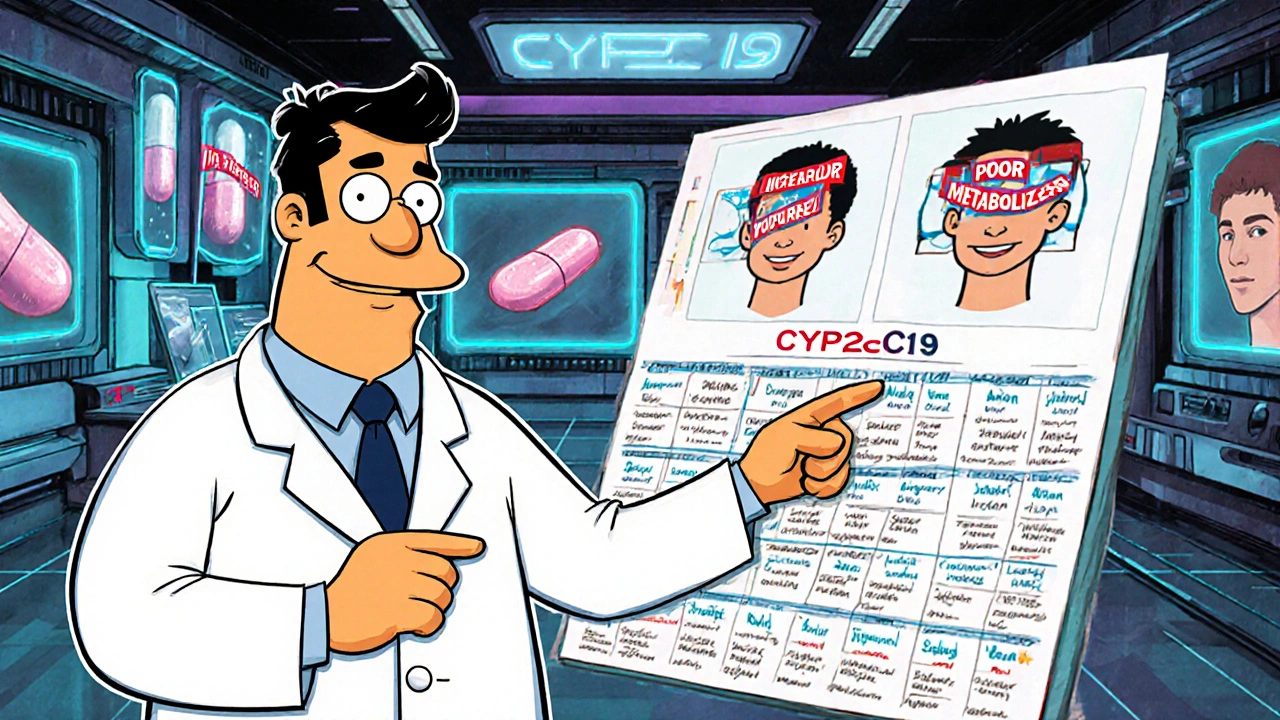
Another key factor: genetics. In Asian populations, where up to 35% of people carry a CYP2C19 loss-of-function gene, the interaction is far more dangerous. One Korean study found omeprazole cut clopidogrel’s effect by over 50% in these patients. In Caucasians, the drop was closer to 30%.
What Do Guidelines Say?
Despite the mixed outcome data, major medical societies are clear: avoid omeprazole and esomeprazole with clopidogrel.
- The American Heart Association and European Society of Cardiology both recommend against combining clopidogrel with omeprazole or esomeprazole.
- The American College of Gastroenterology says pantoprazole 40mg daily is the preferred PPI in this setting.
- The Clinical Pharmacogenetics Implementation Consortium (CPIC) recommends switching to prasugrel or ticagrelor if you’re a poor metabolizer and need a PPI.
The FDA and EMA both list warnings on clopidogrel labels about omeprazole reducing its effectiveness. The FDA specifically mentions 80mg omeprazole reduces clopidogrel’s active metabolite by 45%.
Timing Doesn’t Help
You might think, “What if I take clopidogrel in the morning and omeprazole at night?” It seems logical. But it doesn’t work. CYP2C19 inhibition isn’t about timing-it’s about how long the drug stays in your system. Omeprazole sticks around long enough to block the enzyme all day, no matter when you take your pills. A 2013 study confirmed this: separating doses made zero difference.
What Should You Do?
If you’re on clopidogrel and need acid protection:
- Avoid omeprazole and esomeprazole. They’re the biggest risk.
- Use pantoprazole instead. It’s the safest PPI option.
- Consider rabeprazole if pantoprazole isn’t available or causes side effects.
- Ask about H2 blockers. Famotidine doesn’t affect CYP2C19 and can be used for short-term acid control.
- Ask about genetic testing. If you’ve had a stent or a clot while on clopidogrel, CYP2C19 testing can tell you if you’re a poor metabolizer. If you are, switch to ticagrelor or prasugrel-both work without needing CYP2C19.
And if you’re already taking omeprazole with clopidogrel? Don’t stop either drug on your own. Talk to your doctor. They can switch you to a safer PPI or adjust your antiplatelet therapy.
The Bigger Picture
This interaction isn’t just about two drugs. It’s a window into how personalized medicine is changing cardiology. We used to treat everyone the same. Now we know that your genes, your metabolism, and your drug choices all interact in complex ways.
Since the FDA warning in 2009, prescriptions for omeprazole with clopidogrel dropped by 65% in the U.S. Pantoprazole use rose by 42%. That’s real-world behavior changing because of evidence.
And it’s not over. New PPIs like ilaprazole are being studied, and next-gen antiplatelets are in development to avoid CYP2C19 entirely. By 2025, more cardiology clinics are doing routine genetic testing. That’s the future: no more guessing. Just data-driven choices.
Frequently Asked Questions
Can I take omeprazole with clopidogrel if I only take it occasionally?
No. Even occasional use of omeprazole can inhibit CYP2C19 long enough to reduce clopidogrel’s effectiveness. The inhibition isn’t just about daily dosing-it’s about the drug’s half-life and enzyme binding. If you need stomach protection, switch to pantoprazole or another safer alternative.
Is pantoprazole really safe with clopidogrel?
Yes. Multiple studies show pantoprazole has minimal impact on clopidogrel’s active metabolite levels. At 40mg daily, it reduces exposure by only 14%, which is not considered clinically significant. It’s the recommended PPI in guidelines from the American College of Gastroenterology and others.
Should I get tested for CYP2C19 gene variants?
If you’ve had a stent, heart attack, or stroke while on clopidogrel, or if you’re from an Asian background (where 30-35% of people are poor metabolizers), testing is strongly recommended. If you’re a poor or intermediate metabolizer, clopidogrel may not work well for you-even without omeprazole. Switching to ticagrelor or prasugrel can improve outcomes.
What if I can’t afford ticagrelor or prasugrel?
Cost is a real issue. If you can’t switch to a newer antiplatelet and you need a PPI, pantoprazole is your best option. Some insurance plans cover generic pantoprazole at low cost. Also, ask your doctor about H2 blockers like famotidine for short-term use. Never stop clopidogrel without medical advice.
Are there any natural alternatives to PPIs for acid reflux?
There are no proven natural alternatives that match PPIs in strength or reliability. Lifestyle changes-like avoiding late meals, losing weight, and cutting caffeine-help, but they won’t fully replace medication if you have severe reflux or ulcers. Don’t risk stopping your PPI without a plan. Talk to your doctor about safer options like pantoprazole instead.



Bart Capoen
October 29, 2025so omeprazole and clopidogrel dont mix huh? i had no idea. just switched to pantoprazole last week after my cardiologist said 'dude stop it' lol. been fine since. no more heartburn either. weird how your body just adapts.
Patrick Dwyer
October 31, 2025the CYP2C19 inhibition kinetics are well-documented in the literature-omeprazole is a competitive inhibitor with a Ki in the low micromolar range, effectively saturating the enzyme’s active site. This isn't just pharmacokinetic noise; it's a clinically significant reduction in the formation of clopidogrel’s active thiol metabolite. The 32–49% reduction in AUC is corroborated by multiple pharmacodynamic studies measuring ADP-induced platelet aggregation. The real issue? Most clinicians still default to omeprazole because it's cheap and OTC. We need better education-and mandatory EHR alerts.
Linda Patterson
October 31, 2025Why are we letting big pharma dictate our prescriptions? Omeprazole’s been around for 30 years. Pantoprazole? A corporate invention. The FDA’s warning? A tactic to push expensive alternatives. My grandpa took omeprazole with clopidogrel for 8 years and never had a clot. You think genetics matter? Maybe your genes are just weak. Stop overcomplicating things with your lab reports.
Jen Taylor
November 2, 2025OMG I’m so glad I found this post!! I’ve been on clopidogrel since my stent in 2021, and my GI doc just switched me from omeprazole to pantoprazole last month-my stomach’s been calm, and my cardiologist said my platelet reactivity tests are now in the sweet spot!! I even told my mom, who’s on both meds, and she’s switching too!! 🙌 You guys are lifesavers!!
Shilah Lala
November 3, 2025So basically, if you're not rich, you're supposed to die of a clot because the pharma bros don't want you taking cheap pills? Brilliant. Let me guess-next they'll tell us to stop breathing because oxygen interferes with some expensive new drug.
Christy Tomerlin
November 4, 2025Everyone’s acting like pantoprazole is magic. But have you checked the price? It’s 3x more than omeprazole. And guess what? In 90% of cases, people don’t even need a PPI. Just eat less pizza and stop lying down after dinner. Maybe your acid reflux isn’t a disease-it’s a lifestyle problem.
Susan Karabin
November 4, 2025It’s funny how we treat drugs like they’re separate from our bodies. But they’re not. They’re part of a dance-your genes, your liver, your gut, your habits. Omeprazole isn’t evil. It’s just loud. It’s taking the mic when clopidogrel’s trying to sing. Maybe the real question isn’t which drug to pick-but how to listen better to what our bodies are telling us
luna dream
November 5, 2025Wait… if they’re monitoring CYP2C19, then what’s stopping them from tracking your DNA in your insurance records? Next thing you know, they’ll deny you coverage because you’re a 'poor metabolizer'. They’re already using this to push expensive drugs. This isn’t medicine-it’s a surveillance system with a stethoscope.