Opioid Overdose Recognition Quiz
How well do you know the signs of opioid overdose?
This quiz tests your knowledge of opioid overdose signs and emergency response steps. Try to answer correctly to increase your confidence in recognizing and responding to an overdose situation.
Question 1
Which of these is a key sign of opioid overdose?
Question 2
What should you do immediately if you suspect an opioid overdose?
Question 3
How long does naloxone typically take to work when administered correctly?
Question 4
What happens after naloxone is administered and the person wakes up?
Question 5
What is a common reason for needing multiple naloxone doses?
Quiz Results
Here's how you did:
Knowledge is power. The more you know, the better prepared you are to respond to an opioid overdose emergency. Remember:
- Call 911 immediately
- Administer naloxone if available
- Stay with the person until help arrives
- Medical evaluation is always necessary
Opioid Overdose is a life-threatening condition where opioids suppress the brain's breathing control center. This leads to dangerously slow or stopped breathing, causing oxygen deprivation. Without immediate action, brain damage or death can occur within minutes. According to the CDC, 187 Americans die from drug overdoses every day, with opioids involved in over 80% of those deaths. Knowing the opioid overdose signs is the first step in saving a life.
Key Signs to Watch For
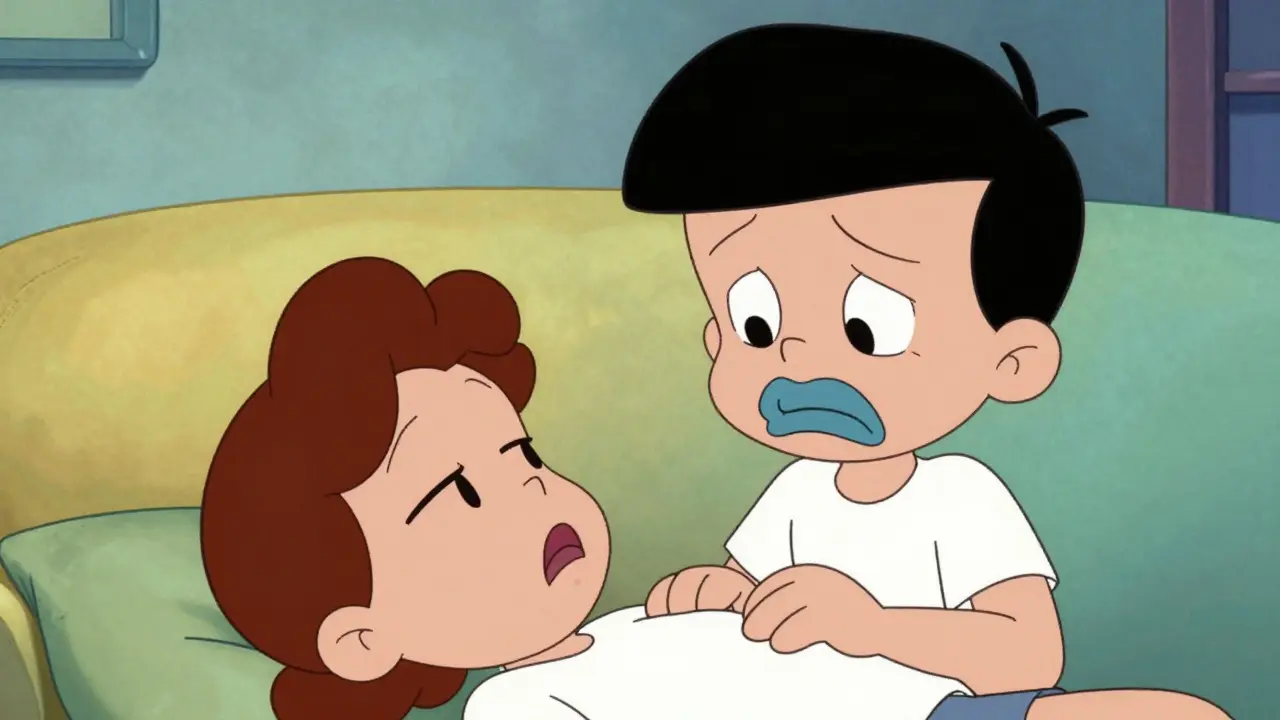
When someone is overdosing, they may show several clear symptoms. The classic triad includes pinpoint pupils, unconsciousness, and slow breathing-but not all signs appear in every case. Here's what to look for:
- Unresponsiveness: The person won't wake up, even when shaken or shouted at. This is often the first sign people notice.
- Pinpoint pupils: Extremely small pupils that don't react to light. However, this isn't always present, especially with certain opioids or stimulant mixtures.
- Blue or purple lips/nails: Known as cyanosis, this happens when oxygen levels drop. Skin may also appear pale or ashen.
- Slow or shallow breathing: Fewer than 12 breaths per minute, or irregular gasping sounds. Sometimes called 'agonal breathing'-this is a sign of respiratory failure.
- Cold, clammy skin: Skin feels cool and sweaty, even if the person is in a warm environment.
Other possible signs include choking or gurgling noises, limp body posture, or confusion before losing consciousness. Remember, if you're unsure, act fast-delaying could cost a life.
Immediate Emergency Steps
Time is critical. The first thing you must do is call 911 immediately. Even if you plan to give naloxone, emergency responders need to know the situation. When you call, tell them exactly what you're seeing-like 'unresponsive person with slow breathing'-so they can prepare. Do not wait to see if the person wakes up on their own. Every minute counts.
Next, if Naloxone is available, administer it right away. Naloxone works quickly to reverse opioid effects, but it's not a substitute for medical care. The CDC emphasizes: 'Overdose deaths are preventable with prompt action.' Stay with the person until help arrives. Your presence can keep them safe while waiting for professionals.
How to Use Naloxone Correctly
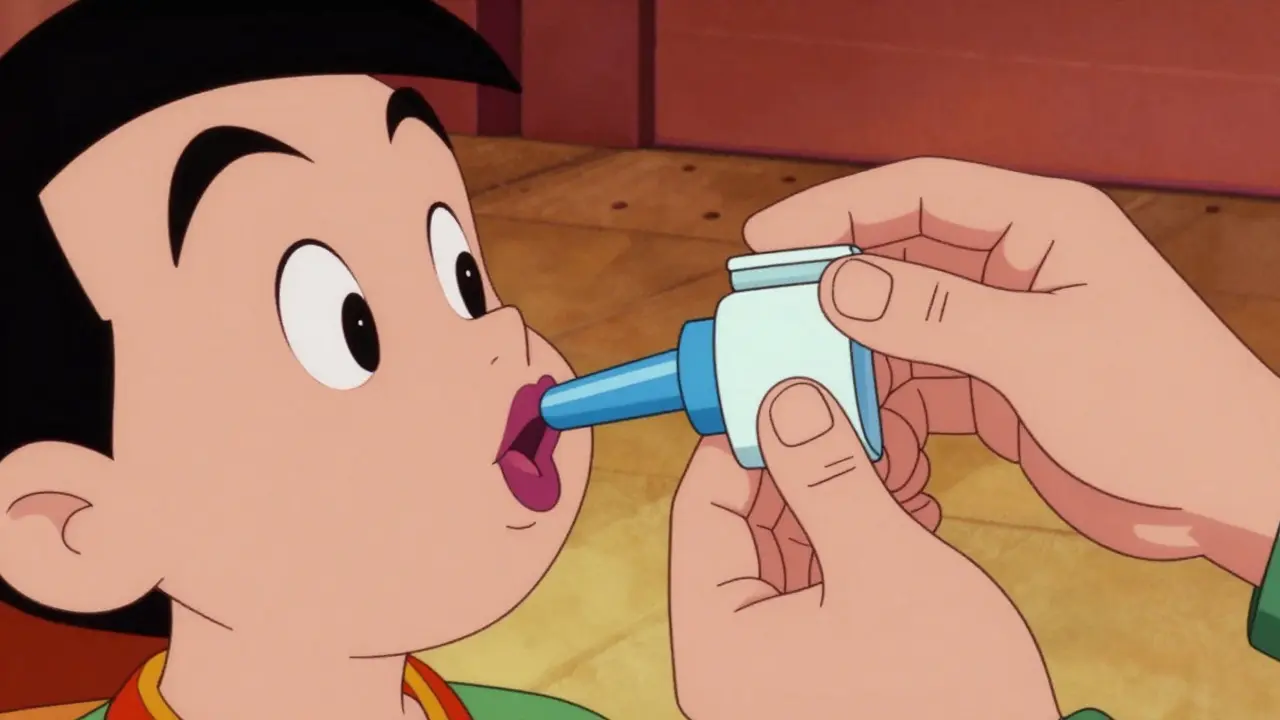
Most naloxone today comes as an intranasal spray (like Narcan). Here's how to use it:
- Remove the cap from the spray nozzle.
- Place the nozzle in one nostril of the person.
- Press the plunger firmly to deliver the full dose.
- If needed, give a second dose in the other nostril after 2-3 minutes.
Naloxone typically starts working in 2-5 minutes. If the person doesn't respond, give another dose. Keep in mind that naloxone's effects wear off in 30-90 minutes. Opioids can stay in the system longer, so the person may need multiple doses. Always call 911-even if they wake up-because they could relapse into overdose later.
Importantly, naloxone is safe. It won't harm someone who hasn't taken opioids. If you're unsure, administer it anyway. As Canada's Health Department states: 'Administer naloxone even if you're in doubt.'
What Happens After Administering Naloxone
After giving naloxone, the person may wake up quickly. But this doesn't mean they're out of danger. Here's what to do next:
- Keep them awake and breathing. Talk to them gently to stay engaged.
- Monitor their breathing closely. If it slows again, prepare to give another naloxone dose.
- Stay with them until emergency responders arrive. They need medical evaluation even after revival.
Many people mistakenly think they're safe once revived. But opioids can re-enter the system after naloxone wears off. In fact, the CDC warns that 'naloxone can wear off before the person has completely recovered from their overdose.' That's why medical professionals must assess them. Also, check for injuries from falls or seizures during the overdose.
Preventing Future Overdoses
Surviving an overdose is just the start. Preventing future incidents requires ongoing support. Here are key strategies:
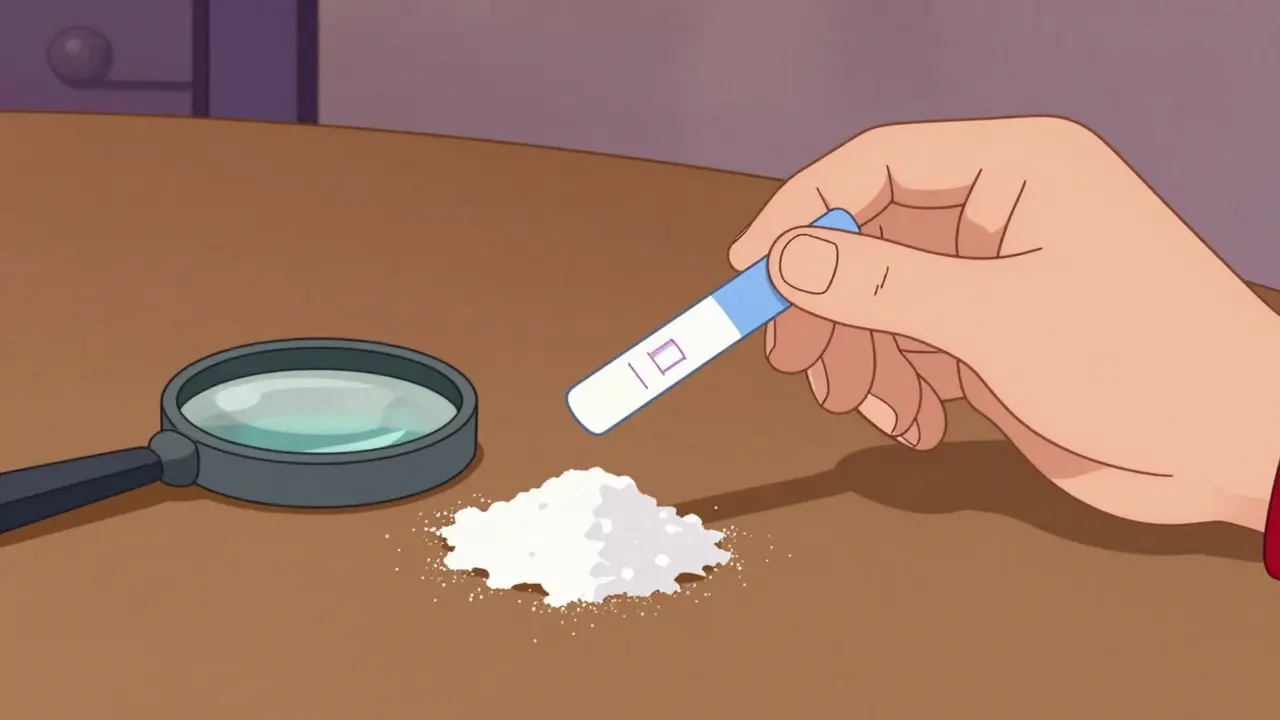
- Fentanyl test strips: These cheap strips can check if drugs contain fentanyl. Many illicit pills and powders are laced with fentanyl, which is 50x stronger than heroin. Using test strips reduces risk significantly.
- Medical treatment: Opioid use disorder (OUD) is a medical condition. Treatment options like medication-assisted therapy (MAT) with buprenorphine or methadone can help manage addiction safely.
- Harm reduction: Programs like needle exchanges and supervised consumption sites reduce overdose risks. They also connect people to treatment and support services.
- Open conversations: Talk to healthcare providers about pain management alternatives. Many overdoses start with prescription opioids. Discussing safer options early can prevent misuse.
Communities with naloxone distribution programs see 14% lower overdose death rates. Public health efforts like these save lives. The CDC's 2023 Overdose Prevention Strategy focuses on expanding access to naloxone, testing, and treatment. Every action matters.
Frequently Asked Questions
Can naloxone be used on someone who hasn't taken opioids?
Yes, naloxone is safe to use even if opioids aren't involved. It only works on opioid receptors, so it won't harm someone who hasn't taken opioids. Health authorities like the CDC and Canada's Health Department recommend administering naloxone 'even if you're in doubt' because the risks of not acting far outweigh any potential side effects.
What if I'm not sure if it's an opioid overdose?
Act immediately. The signs of opioid overdose-like unresponsiveness, slow breathing, and blue lips-are distinct. If you suspect an overdose, call 911 and give naloxone. Delaying action could be fatal. Remember, naloxone is safe to use even if opioids aren't present, so there's no downside to acting quickly.
How long does naloxone take to work?
Naloxone typically starts working within 2-5 minutes when given intranasally or intramuscularly. However, its effects last only 30-90 minutes, which is often shorter than the opioids in the system. This means the person may need multiple doses. Always stay with them until emergency help arrives.
Can naloxone be used on children?
Yes, naloxone is safe for children of all ages. The dosage is based on body weight, but in an emergency, giving the standard dose is better than waiting. Pediatric emergency guidelines confirm naloxone is appropriate for suspected opioid overdoses in kids. Always call 911 immediately after administering.
What should I do after the person wakes up?
Even if they seem fine, they need medical evaluation. Opioids can re-enter the bloodstream after naloxone wears off, causing a second overdose. Stay with them until EMS arrives, and encourage them to seek treatment for opioid use disorder. Follow-up care is critical for long-term recovery.




Bella Cullen
February 5, 2026Always call 911 first, even if you have naloxone.
Matthew Morales
February 6, 2026Yeah, that's right! I've seen people hesitate to call 911 because they're scared of legal trouble. but it's better to call than let someone die 😬. also, naloxone is safe to use even if you're not sure.
Carl Crista
February 8, 2026Fentanyl is everywhere now. Even pills that look like oxycodone are fentanyl. You need test strips. Don't trust what you think you have. Always test.
Diana Phe
February 9, 2026Test strips? That's a government ploy. They want to control us. But I've heard they're fake. Don't trust them.
Rene Krikhaar
February 10, 2026Opioid use disorder is a medical condition, not a moral failing. Treatment like buprenorphine or methadone works. People need help, not judgment. MAT saves lives. I've worked in addiction medicine for years. The stigma is the biggest barrier. People don't seek help because they're afraid of being labeled. Medication-assisted therapy isn't just replacing one drug with another. It's stabilizing the brain. It allows people to function, hold jobs, and rebuild their lives. Studies show MAT reduces overdose deaths by up to 50%. It's one of the most effective tools we have. But access is limited. Insurance doesn't always cover it. Doctors need more training. We need to expand treatment options. If you or someone you know is struggling, please reach out. There's hope. Recovery is possible.
Samantha Beye
February 10, 2026Exactly. I've seen people recover with MAT. It's not just about stopping drugs; it's about managing the condition like diabetes or hypertension. The key is consistent treatment and support.
one hamzah
February 10, 2026Fentanyl test strips are a game-changer! 🔥 They're cheap and easy to use. Always check before using any substance. Harm reduction is key. Stay safe! 💯 I've been using them for months now. They're super simple. Just a tiny bit of the drug mixed with water, then dip the strip. If it's positive, don't use it. Fentanyl is sneaky. It's in so many pills and powders. You never know what you're getting. Test strips can save your life. The government should make them more available. Everyone should have access. It's not about judging people; it's about keeping them alive. I've seen friends overdose because they didn't know there was fentanyl. If they had tested, they'd be here. It's not just about opioids. Cocaine and meth are being laced with fentanyl too. So test strips work for everything. The harm reduction community is doing amazing work. We need more support. Don't be afraid to ask for help. Talk to your friends. If someone uses, encourage them to test. It's not about being perfect. It's about making safer choices. I've had my own struggles. Test strips helped me stay safe. Please, if you use drugs, get a test strip. It's a small step that could save your life. The CDC says fentanyl is the leading cause of overdose deaths. We need to fight it. Education is key. Share this info. Let's save lives together. Stay safe out there. 💙
Dr. Sara Harowitz
February 12, 2026Yes! Test strips are essential! But people need to stop using drugs altogether. Addiction is a choice! And the government should crack down harder on dealers.
Georgeana Chantie
February 13, 2026Naloxone is overrated. People should just tough it out. Why are we enabling drug users? 🤷♀️
Sam Salameh
February 14, 2026Hey, I get where you're coming from, but naloxone saves lives. It's not about enabling; it's about giving people a chance to get help. We need to help each other.
Jennifer Aronson
February 16, 2026The CDC's 2023 strategy emphasizes expanding naloxone access and treatment. Public health efforts like needle exchanges reduce overdose deaths significantly.
Phoebe Norman
February 16, 2026Needle exchanges are a necessary evil. They connect people to care. But the real issue is the pharmaceutical industry's role in the opioid crisis. Big Pharma pushed opioids on doctors.
Carl Crista
February 16, 2026Big Pharma is a conspiracy. They control everything. Even naloxone is part of the plan. Don't trust the system.