
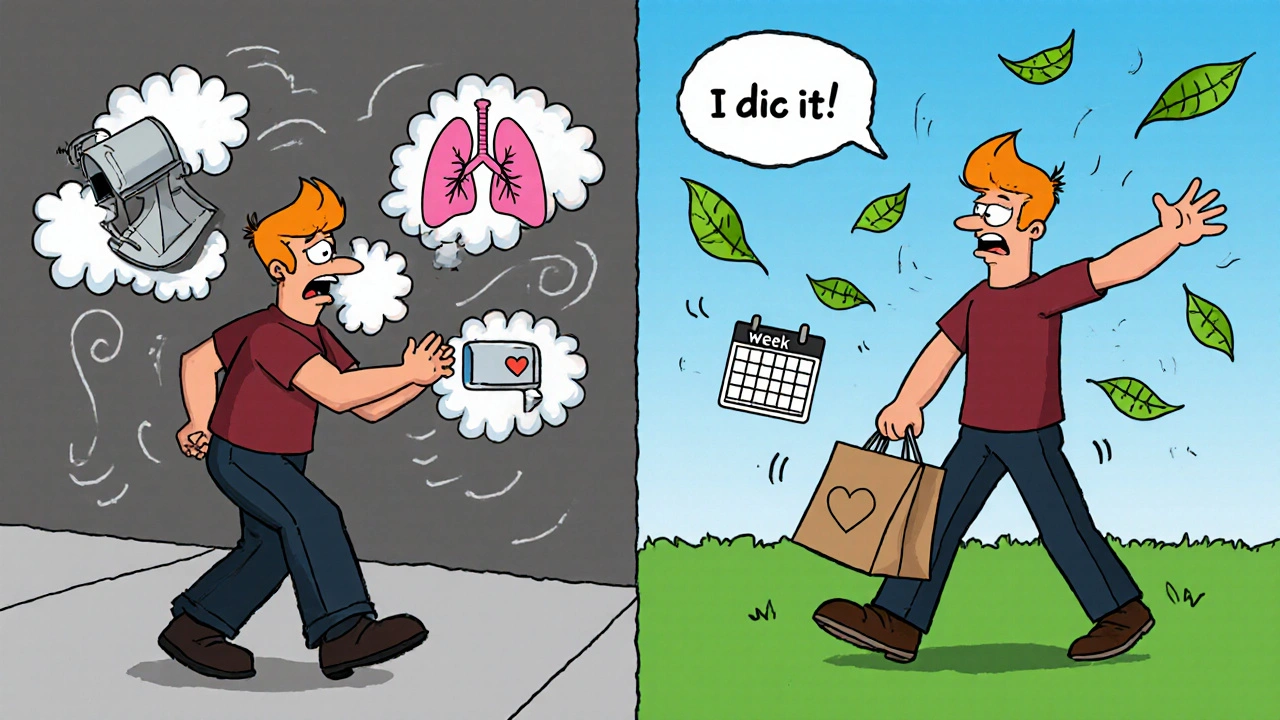
When you have a chronic lung disease like COPD, interstitial lung disease, or bronchiectasis, everyday tasks-walking to the mailbox, climbing stairs, even showering-can leave you breathless and exhausted. Medications help, but they don’t fix the muscle weakness, the fear of breathing, or the isolation that comes with it. That’s where pulmonary rehabilitation steps in. It’s not a magic cure, but it’s one of the most effective, evidence-backed tools you can use to take back control of your life.
What Exactly Is Pulmonary Rehabilitation?
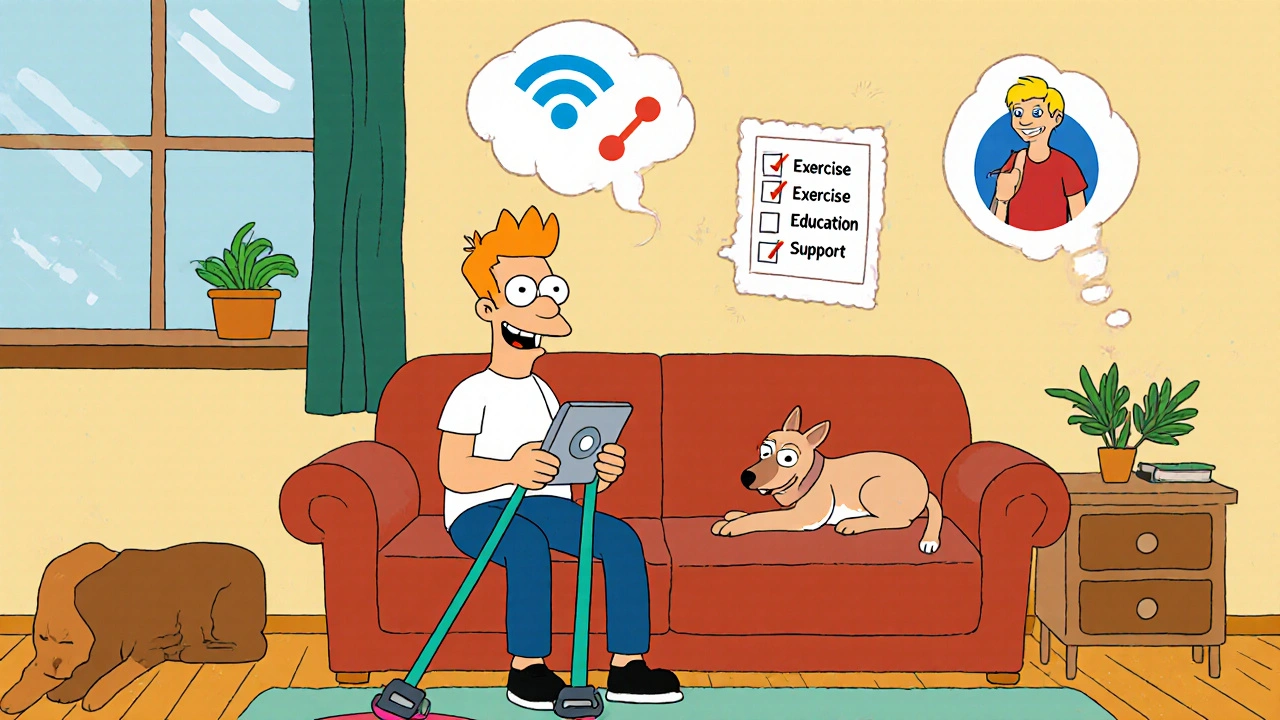
Pulmonary rehabilitation (PR) is a structured, supervised program designed for people with long-term lung conditions. It’s not just exercise. It’s not just education. It’s both-plus emotional support, nutrition advice, and practical strategies to manage symptoms day to day. According to the 2023 guidelines from the American Thoracic Society and European Respiratory Society, PR is defined as a comprehensive intervention that starts with a full assessment and then builds a personalized plan to improve your physical strength, reduce breathlessness, and boost your overall quality of life.
It’s been around since the early 2000s, but it’s only in the last decade that it’s become a true standard of care-not just for COPD, but for a wide range of chronic lung diseases. Whether you’ve been diagnosed with pulmonary hypertension, cystic fibrosis, or are recovering from a lung transplant, PR can help if your symptoms are limiting your daily activities.
The Four Core Pieces of Pulmonary Rehabilitation
Every effective PR program has four key parts. Skip any one, and you’re missing out on the full benefit.
- Exercise Training: This is the engine of PR. It’s not about running marathons. It’s about rebuilding strength in your legs, arms, and breathing muscles. Most programs include aerobic training-like walking on a treadmill or using a stationary bike-at a pace that challenges you but doesn’t overwhelm you. You’ll also do resistance training with light weights or resistance bands to strengthen your arms and core. Sessions are usually 60 to 90 minutes, two or three times a week, for 6 to 12 weeks. Studies show people gain an average of 38.5 meters on the 6-minute walk test after completing PR. That might not sound like much, but for someone who used to stop every 50 feet, it means walking to the corner store without needing to rest.
- Education: You’ll learn how your lungs work (or don’t work), how your medications really help, and how to spot the early signs of a flare-up. Knowing when to call your doctor instead of waiting until you’re in crisis can prevent hospital visits. Many patients say this part changed everything-they finally understood why they felt the way they did.
- Behavior and Mindset Support: Chronic lung disease doesn’t just affect your body. It wears you down emotionally. Anxiety about breathing, depression from isolation, and frustration over lost independence are common. PR programs include psychologists or counselors who help you cope. Group sessions also build community. You’re not alone. Others get it.
- Assessment and Tracking: Before you start, you’ll be tested: lung function, how far you can walk in six minutes, your quality of life score. At the end, you’re tested again. This isn’t just paperwork-it’s proof of progress. And seeing that improvement? It’s powerful.
Who Can Benefit From Pulmonary Rehabilitation?
PR isn’t just for people with severe COPD. The 2023 guidelines say it’s for anyone with a chronic lung disease who feels limited by their symptoms-even if your lung function test looks “mild.”
Here’s who it helps most:
- COPD (all stages): Especially stages 2 to 4. People with severe COPD see the biggest jump in walking distance and fewer hospital visits.
- Interstitial Lung Disease (ILD): Studies show improved breathing and less fatigue after PR, even though the lung scarring doesn’t go away.
- Pulmonary Hypertension: While evidence is still growing, PR helps with stamina and reduces dizziness during activity.
- Bronchiectasis: PR helps clear mucus better and reduces infections over time.
- Cystic Fibrosis: Especially for teens and adults, PR improves strength and endurance as the disease progresses.
- Before and After Lung Transplant: Pre-op PR builds strength so you recover faster. Post-op PR helps you regain independence.
Even if you’ve been told “there’s nothing more we can do,” PR is still an option. It’s not about curing the disease-it’s about helping you live better with it.
How Does PR Compare to Just Taking Medication?
Medications like inhalers and bronchodilators are essential. But they don’t rebuild your muscles or teach you how to breathe more efficiently. A 2023 review compared PR to common COPD drugs and found something surprising: PR was better.
For example:
- PR improved exercise capacity by 0.91 effect size. Bronchodilators? Only 0.41.
- PR reduced breathlessness (dyspnea) by 0.82 effect size. Medications? Just 0.35.
- Quality of life scores jumped 0.78 with PR. With drugs alone? 0.38.
One study showed that people in PR improved their endurance time on a treadmill by 152%. Those on tiotropium (a common inhaler) only improved by 26%. PR doesn’t replace meds-it makes them work better by strengthening your body’s response.
Where and How Is PR Delivered?
Most PR programs run in outpatient clinics-hospitals, rehab centers, or dedicated lung health facilities. But things are changing.
Today, you have options:
- In-person: 78% of programs still happen in clinics. You get direct supervision, access to equipment, and real-time feedback.
- Home-based: 5% of programs are fully home-based. You get a kit with weights, a pulse oximeter, and a workout plan. A nurse checks in weekly.
- Telehealth: This is the fastest-growing option. In 2023, 12% of programs were delivered via video calls. A recent JAMA trial found telehealth PR was just as effective as in-person for improving walking distance and breathlessness. This is huge for people in rural areas or with mobility issues.
Programs usually last 6 to 12 weeks, but some go longer-up to 24 months-for people who need ongoing support. The key is consistency. Missing more than two sessions a week reduces your gains.
Real People, Real Results
Numbers are important, but stories stick.
A 68-year-old man in Cleveland, diagnosed with GOLD stage 3 COPD, could barely walk 182 meters on the 6-minute walk test before PR. After 12 weeks, he walked 327 meters. For the first time in five years, he went grocery shopping on his own.
On Reddit, a user named u/BreathingEasy shared: “After 8 weeks of PR, I went from needing oxygen at 1L to being off oxygen during daily activities.”
A 2022 survey of 127 PR participants found that 89% said their most meaningful improvement was “walking to the mailbox without stopping.” That’s not a lab result. That’s freedom.
People report better sleep, less anxiety, more confidence, and even renewed social lives. One woman started joining her book club again. Another began gardening. These aren’t side effects-they’re the point.
Barriers to Getting Started
PR works-but most people who need it never get it.
Here’s why:
- Access: Only 57% of U.S. counties have a certified PR program. If you live in a rural area, you might be 50 miles from the nearest clinic.
- Referral: Many doctors don’t know to refer patients. Only 10-15% of eligible COPD patients in the U.S. actually enroll.
- Cost and Coverage: Medicare covers 36 sessions per year, but you need a doctor’s note proving medical necessity. Some private insurers are slower to cover it. And even with coverage, you might pay for transportation, parking, or time off work.
- Perception: Some people think, “I’m too weak to exercise.” But PR starts where you are. If you can sit up, you can start.
The good news? Telehealth is breaking down many of these barriers. If you can’t get to a clinic, ask your doctor about a home or virtual program.
How to Get Started
Here’s what to do:
- Talk to your doctor. Say: “I’m struggling with daily activities because of my lung disease. Is pulmonary rehabilitation right for me?”
- Ask for a referral. If they say no, ask why. If they’re unsure, suggest the 2023 ATS/ERS guidelines.
- Check local programs. The American Lung Association’s Lung HelpLine (1-800-LUNGUSA) can help you find one near you.
- Ask about telehealth. If travel is hard, ask if they offer virtual sessions.
- Commit to the first 4 weeks. The first few sessions are the hardest. But most people feel a difference by week 6.
You don’t need to be “strong enough.” You just need to be willing to try.
What Happens After the Program Ends?
PR isn’t a one-time fix. It’s a launchpad. The goal is to keep moving, keep breathing well, and keep managing your condition long after the supervised sessions end.
Most programs give you a home exercise plan. Some offer maintenance groups once a week. Others connect you with online communities like the Pulmonary Wellness Foundation, which has over 15,000 members.
The key is consistency. Even 20 minutes of walking or light resistance training three times a week can keep your gains. And if you feel yourself slipping-more breathlessness, less activity-don’t wait. Go back. Re-enroll. PR is something you can return to as often as you need.
The Bigger Picture
Chronic lung diseases affect over half a billion people worldwide. In the U.S. alone, 16.4 million have COPD-but only 3.2% complete a full PR program. That’s not because PR doesn’t work. It’s because systems aren’t built to deliver it.
But change is happening. More hospitals are offering PR. Telehealth is expanding access. Insurance coverage is slowly improving. And the evidence keeps growing: PR reduces hospital readmissions by 32%, improves survival, and gives people back their lives.
If you or someone you love has a chronic lung condition, PR isn’t a last resort. It’s the most powerful, practical tool you have to live better-today and for years to come.
Is pulmonary rehabilitation only for people with COPD?
No. While COPD is the most common reason people join, PR is now recommended for anyone with a chronic lung disease who feels limited by symptoms. This includes interstitial lung disease, pulmonary hypertension, bronchiectasis, cystic fibrosis, and people preparing for or recovering from lung transplants. The 2023 guidelines expanded eligibility to include all chronic respiratory conditions with functional limitations-not just based on lung test scores.
How long does it take to see results from pulmonary rehabilitation?
Most people start noticing improvements within 4 to 6 weeks. You might feel less breathless climbing stairs, or be able to walk farther without stopping. By the end of a typical 8- to 12-week program, studies show measurable gains in walking distance, muscle strength, and quality of life. The biggest changes often come between weeks 6 and 10, when your body starts adapting to the training and your confidence grows.
Does Medicare cover pulmonary rehabilitation?
Yes. Medicare covers up to 36 sessions of pulmonary rehabilitation over your lifetime, with the option to extend to 72 sessions if your doctor documents medical necessity. Coverage includes exercise training, education, and monitoring. You’ll need a referral from your doctor, and the program must be provided by a certified facility. Most programs handle the billing for you, but it’s good to confirm coverage before starting.
Can I do pulmonary rehabilitation at home?
Yes, and it’s becoming more common. Home-based PR programs provide you with equipment like resistance bands, a pulse oximeter, and a personalized exercise plan. You’ll have regular check-ins with a therapist via phone or video. A 2023 study found home-based PR delivered results just as strong as in-person programs for walking distance and breathlessness. This option is ideal if you live far from a clinic, have trouble traveling, or prefer the comfort of home.
What if I’m too weak to exercise?
PR starts where you are-even if you can only sit in a chair. Therapists use low-intensity exercises like seated leg lifts, arm circles, or breathing techniques to begin building strength. For those who are very deconditioned, neuromuscular electrical stimulation (NMES) can help activate muscles without requiring movement. The goal isn’t to push you to exhaustion. It’s to help you slowly regain the ability to do daily tasks without getting winded.
Will pulmonary rehabilitation cure my lung disease?
No. PR doesn’t reverse lung damage from COPD, scarring, or other chronic conditions. But it doesn’t need to. Its goal is to help your body work better with what you have. By strengthening your muscles, improving your breathing technique, and teaching you how to manage symptoms, PR lets you live more fully despite the disease. Many people say it feels like getting their life back-not because their lungs changed, but because their ability to move and function did.



Robert Merril
November 16, 2025PR works but good luck getting your doctor to refer you theyd rather just write another script
Kathy Grant
November 18, 2025I was told I was too weak to start exercise. Then I did seated arm circles for 5 minutes twice a day. Six weeks later I walked to the end of my driveway without stopping. It wasn’t magic. It was just consistent tiny efforts. I cried the first time I carried my own groceries. No one talks about that part-the quiet victories.
Georgia Green
November 18, 2025my doc said i qualified but the nearest program is 90 mins away and i dont drive anymore. telehealth saved me. i did it from my couch with resistance bands and a pulse ox. lost 12lbs and stopped needing o2 during meals. thanks for the info
Margo Utomo
November 20, 2025PR is literally the only thing that didn’t make me want to die. 🥹 I went from crying in the shower to gardening again. Also I bought myself a tiny plant called Barry. He’s thriving. I’m thriving. 🌱💪
Roberta Colombin
November 21, 2025Everyone deserves access to this. No one should be told they are too sick to try. The fact that only 57% of counties have programs is a failure of our system. Not a reflection of need.
Noel Molina Mattinez
November 21, 2025you think this is new? i did this in 2008. they called it rehab then. now its PR. same thing. they just repackaged it and raised the price
George Gaitara
November 21, 2025they say PR reduces hospital visits by 32% but did they account for the fact that people who do PR are the ones who already care enough to show up? of course it works for them. the people who need it most never even try
Sylvia Clarke
November 22, 2025Let’s be honest-this isn’t about health. It’s about control. The medical industrial complex doesn’t profit from rehab. It profits from inhalers, ER visits, and oxygen tanks. PR is inconvenient. It requires human interaction. It doesn’t scale. So they let it languish. And we’re told it’s our fault we’re too weak to walk.
Eva Vega
November 24, 2025From a pulmonary physiology standpoint, the neuromuscular adaptations observed in PR are primarily mediated through increased type I fiber recruitment and improved ventilatory efficiency. The 6-minute walk test improvements correlate strongly with reduced ventilatory equivalents for CO2, suggesting enhanced peripheral muscle oxygen utilization rather than pulmonary improvement.
Ashley Unknown
November 25, 2025Did you know the pharmaceutical companies funded the 2023 guidelines? They wanted to make sure PR looked good so they could sell more meds to people who failed PR. I know a guy who got kicked out of his program because he asked too many questions. They said he was "non-compliant." He was just trying to find out who really owns the rehab centers. I’m not saying it’s a conspiracy. I’m just saying… why is the CEO of one of the biggest PR chains also on the board of a major inhaler manufacturer?
Jennifer Howard
November 26, 2025It's not that PR doesn't work-it's that people who do it are the ones who still have the will to live. Those of us who are truly suffering? We're the ones who've given up. We don't have the energy to drive to a clinic. We don't have the emotional bandwidth to pretend we're okay. And frankly, we're tired of being told to "just try harder."
Christina Abellar
November 26, 2025My mom did PR after her transplant. She started with breathing exercises in a chair. Now she walks 2 miles every morning. It’s not about curing. It’s about living. Thank you for writing this.
Matt Wells
November 27, 2025The 2023 ATS/ERS guidelines are flawed. The meta-analyses used to justify PR’s efficacy are plagued by selection bias and lack of long-term follow-up. The effect sizes cited are statistically significant but clinically marginal. One should not mistake statistical significance for meaningful improvement in quality of life.
Dave Feland
November 28, 2025PR is a scam. The government funds it because it’s cheaper than covering lifelong oxygen. They don’t care if you live better-they care if you live longer. And if you die faster? Well, that’s just market correction.
Margo Utomo
November 29, 2025to the person who said "it’s a scam"-you don’t get it. I was on 4L of oxygen just to pee. Now I walk to the mailbox in my slippers. No oxygen. No drama. Just me and my garden. 💚 You don’t have to believe in PR. Just try it. Even once. I dare you.