Medication & Caffeine Timing Calculator
Select a medication to see recommended timing guidelines.
Most people don’t think twice about drinking coffee with their morning pills. But what if that cup of coffee is making your medication less effective-or even dangerous? The truth is, caffeine doesn’t just wake you up. It can interfere with how your body processes at least 127 common medications, from blood thinners to antidepressants to thyroid pills. And the consequences aren’t theoretical. People end up in emergency rooms because they didn’t know that one cup of coffee could spike their heart rate, raise their blood pressure, or make their seizure medication fail.
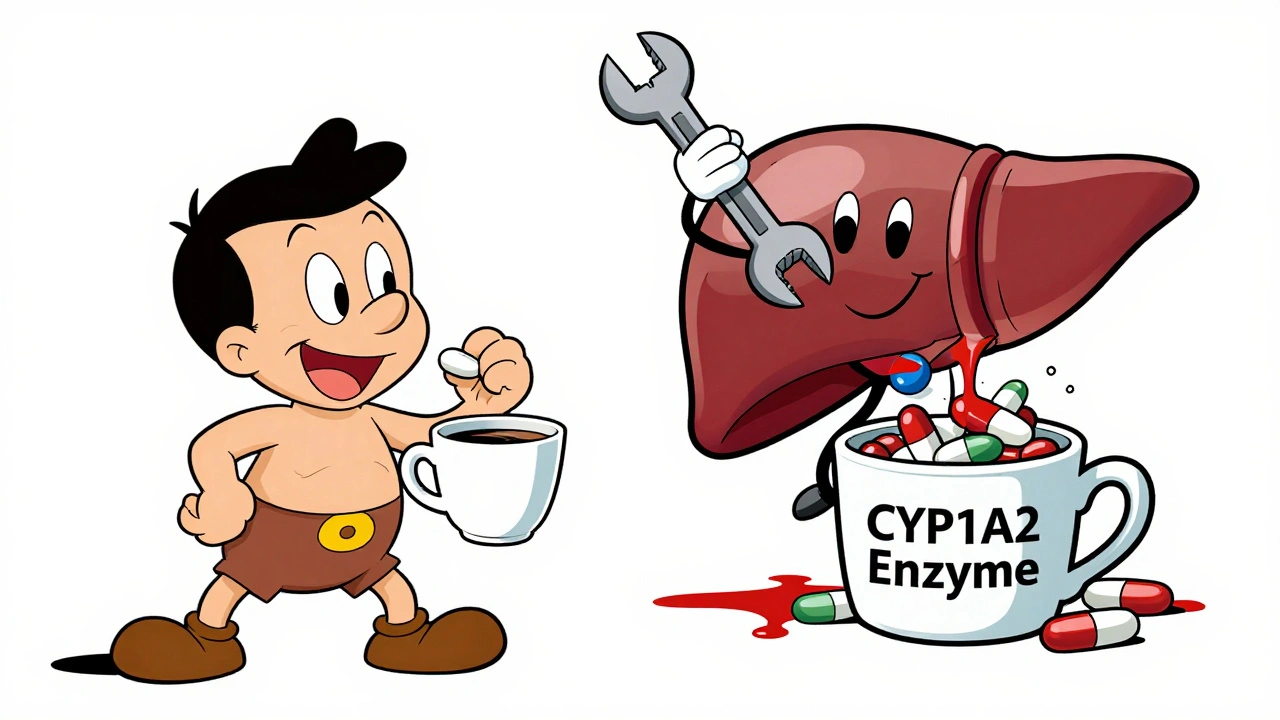
How Caffeine Changes the Way Medications Work
Caffeine isn’t just a stimulant. It’s a powerful player in your liver’s drug-processing system. About 10-15% of all prescription drugs are broken down by an enzyme called CYP1A2. Caffeine blocks that enzyme. When you drink coffee, you’re essentially putting a wrench in the machine that’s supposed to clear those drugs from your body. The result? The medication builds up to higher levels than intended, or it doesn’t get absorbed properly at all.
For example, if you take warfarin (a blood thinner) and drink coffee regularly, your INR levels-the measure of how long it takes your blood to clot-can jump by 15-25% within just 24 hours. That means you’re at higher risk of bleeding. On the flip side, if you suddenly cut back on coffee while staying on the same dose of warfarin, your INR can drop, increasing your risk of clots. Consistency matters more than you think.
It’s not just about liver enzymes. Caffeine also blocks adenosine receptors in your brain and heart. That’s why it keeps you alert. But it’s also why it can make cardiac stress tests useless. Medications like adenosine and dipyridamole rely on activating those same receptors to stress your heart during testing. If caffeine is blocking them, the test won’t work. That’s why cardiologists require you to avoid caffeine for 24 hours before the test. One cup of coffee can ruin the whole procedure.
Thyroid Medication: The Silent Saboteur
If you take levothyroxine (Synthroid, Levoxyl, or generic), your coffee might be quietly sabotaging your treatment. A 2017 study of 98 patients showed that drinking coffee within an hour of taking thyroid medication reduced absorption by 25-57%. That’s not a small drop-it’s enough to push your TSH levels out of range. One patient on Reddit shared that after years of stable TSH at 1.8, it jumped to 4.5 after years of taking Synthroid with coffee. The fix? Waiting 60 minutes after taking the pill before drinking coffee. Simple. Effective. Often ignored.
The Endocrine Society recommends waiting 30 to 60 minutes between taking levothyroxine and consuming anything with caffeine. That includes tea, energy drinks, chocolate, and even decaf coffee-which still contains 2-15 mg of caffeine. For people with hypothyroidism, even that small amount can matter.
Psychiatric Drugs: When Coffee Makes Anxiety Worse
Antidepressants and caffeine don’t mix well-and the risks vary wildly depending on the drug. Fluvoxamine (Luvox) and escitalopram (Lexapro), both SSRIs, are particularly sensitive. Harvard Health found that coffee can reduce fluvoxamine absorption by up to 33%. That means you’re not getting the full dose, and your depression or anxiety symptoms may not improve.
On the other hand, tricyclic antidepressants like amitriptyline and imipramine can become dangerously concentrated in your blood when combined with caffeine. The CYP1A2 enzyme that breaks down these drugs gets blocked, so levels rise by 20-40%. That can lead to dizziness, dry mouth, rapid heartbeat, confusion, and even seizures in extreme cases. A 2024 Drugs.com analysis of over 1,200 users found that 68% of people on psychiatric meds reported worse anxiety when they drank coffee with their pills.
Dr. Robert H. Shmerling from Harvard Health puts it bluntly: “Drinking coffee-especially in large amounts-can affect how your body processes these drugs.” If you’re on antidepressants and suddenly feel more jittery, restless, or wired, coffee might be the culprit-not your mental health.
Heart Medications and Blood Pressure: A Dangerous Combo
Cardiac drugs are among the most sensitive to caffeine. The American Heart Association reports that caffeine-medication interactions contribute to 2.8% of all adverse drug events in adults over 50-and 37% of those require ER visits.
Verapamil, a calcium channel blocker used for high blood pressure and arrhythmias, can be temporarily less effective when paired with caffeine. Mayo Clinic’s 2023 guide shows that blood pressure readings can spike 8-12 mmHg for 2-3 hours after caffeine intake. For someone already struggling with hypertension, that’s enough to trigger a dangerous episode.
And then there’s pseudoephedrine-the decongestant in many cold and allergy meds. When combined with caffeine, it can cause a heart rate increase of 20-35 beats per minute and a systolic blood pressure rise of 15-25 mmHg within 45 minutes. That’s not just uncomfortable. It’s risky for people with heart disease or uncontrolled hypertension. University Hospitals’ 2025 update advises avoiding caffeine for 4-6 hours after taking pseudoephedrine.
Diabetes and Stimulants: Blood Sugar on a Rollercoaster
If you have diabetes, caffeine can throw your blood sugar into chaos-especially when mixed with stimulants like pseudoephedrine. Research shows that combining caffeine with pseudoephedrine can raise blood sugar by 15-25 mg/dL. That’s a big swing for someone managing insulin or oral diabetes meds. Body temperature can also rise by 0.5-1.0°C, adding stress to an already taxed system.
And if you’re taking stimulant ADHD meds like Adderall or Ritalin? Caffeine doesn’t just add to the buzz-it multiplies it. Patients on PatientsLikeMe report being unable to sleep for 12+ hours after taking Adderall with morning coffee. Heart palpitations, shaking, and panic attacks are common complaints. The combination isn’t just unpleasant-it can be medically dangerous.
Seizure Medications: A Risk You Can’t Afford to Ignore
For people with epilepsy, caffeine isn’t just a morning ritual-it’s a potential trigger. Studies in Epilepsy & Behavior found that patients taking carbamazepine, phenytoin, valproate, or other seizure meds had 18-35% more seizures when consuming regular caffeine. Why? Caffeine lowers the seizure threshold. It makes your brain more excitable. Even if you’ve been stable for years, a sudden increase in coffee intake can tip you over the edge.
There’s no safe threshold here. Some patients tolerate small amounts. Others can’t handle even one cup. If you have epilepsy, talk to your neurologist. Don’t assume your dose is set in stone. Your caffeine habits might need to change.
What You Can Do: Simple Rules to Stay Safe
You don’t have to give up coffee. But you do need to manage it wisely. Here’s what works:
- For thyroid meds (levothyroxine): Wait at least 60 minutes after taking your pill before drinking coffee or tea.
- For blood thinners (warfarin): Keep your caffeine intake consistent. Don’t go from 1 cup to 4 cups a day. Stick to under 200 mg daily (about 2 cups of coffee).
- For psychiatric meds: Avoid caffeine entirely if you’re on fluvoxamine or tricyclics. If you’re on SSRIs, monitor your anxiety levels. If it’s worse after coffee, cut back.
- For cardiac stress tests: No caffeine for 24 hours. That includes tea, soda, chocolate, and energy drinks.
- For stimulants (ADHD meds, pseudoephedrine): Don’t combine. If you need a cold remedy, choose a caffeine-free option.
- For seizure meds: Talk to your doctor. Some patients need to eliminate caffeine completely.
And remember: decaf isn’t caffeine-free. It still has enough to affect sensitive medications. If you’re on a high-risk drug, treat decaf like regular coffee.

When to Call for Help
Some reactions need immediate attention. If you experience any of these after drinking coffee with your meds, seek help right away:
- Heart rate over 120 bpm
- Systolic blood pressure above 180 mmHg
- Difficulty breathing
- Confusion, vision changes, or loss of coordination
- Twitching, rigid muscles, or shaking
- Worsening depression or suicidal thoughts
- Seizures or altered mental state
These aren’t side effects you can tough out. They’re warning signs that your body is reacting dangerously to the mix of caffeine and medication.
Why This Isn’t Just a ‘Maybe’ Problem
Here’s the reality: 85% of Americans drink caffeine daily. Nearly half of them take at least one prescription medication. That means over 150 million people are at risk. The American Pharmacists Association estimates these interactions cost the U.S. healthcare system $1.2 billion a year in avoidable ER visits, hospitalizations, and failed treatments.
And it’s getting worse. The FDA added caffeine interaction warnings to 15 new drugs in 2024. Drug databases now flag 127 medications for caffeine interactions-up from 89 in 2020. Hospitals are now using electronic systems to flag these risks automatically. But you can’t rely on the system. You need to know your own risks.
It’s not about fear. It’s about control. You can still enjoy your coffee. But if you’re on medication, you need to treat caffeine like a drug itself-because it is.
Can I drink coffee with my thyroid medication?
No-not right away. Drinking coffee within an hour of taking levothyroxine can reduce absorption by up to 57%. Wait at least 60 minutes after taking your pill before having coffee. This applies to all caffeinated drinks, including tea and energy drinks. Decaf coffee still contains enough caffeine to interfere, so treat it the same way.
Does caffeine affect blood thinners like warfarin?
Yes. Caffeine can increase your INR levels by 15-25% within 24 hours, raising your risk of bleeding. The key is consistency: if you drink coffee every day, keep the amount the same. Don’t suddenly switch from one cup to four. The American Heart Association recommends limiting caffeine to no more than 200 mg per day (about two cups of coffee) if you’re on warfarin.
Is decaf coffee safe with medications?
Not always. Decaf coffee still contains 2-15 mg of caffeine per cup. While that’s low, it’s enough to interfere with sensitive medications like thyroid drugs, antidepressants, or seizure medications. If you’re on one of these, treat decaf like regular coffee and wait the recommended time before consuming it.
Can caffeine make my antidepressant less effective?
It can. Fluvoxamine and escitalopram (Lexapro) are especially affected-coffee can reduce their absorption by up to 33%. Other antidepressants, like amitriptyline, can become too strong when combined with caffeine, increasing side effects like dizziness and rapid heartbeat. If you notice more anxiety, jitteriness, or sleep problems after drinking coffee, it might be the cause.
Why do I need to avoid caffeine before a cardiac stress test?
Because caffeine blocks adenosine receptors, which are the exact targets of the drugs used in stress tests (like adenosine or dipyridamole). If those receptors are blocked, the test won’t work properly. Results can be inconclusive, meaning you’ll have to reschedule. The American College of Cardiology requires 24 hours of caffeine abstinence before the test-no coffee, tea, soda, or chocolate.
What should I do if I accidentally drank coffee with my medication?
If you took your medication and drank coffee within the recommended window, don’t panic. One mistake won’t cause immediate harm in most cases. But monitor yourself for symptoms like rapid heartbeat, dizziness, anxiety, or unusual fatigue. If you’re on a high-risk medication like warfarin, thyroid drugs, or seizure meds, contact your doctor or pharmacist. They may want to check your blood levels or adjust your dose. Going forward, set a reminder to wait the full 30-60 minutes before drinking coffee.
Final Thought: Caffeine Is a Drug Too
You wouldn’t mix alcohol with your prescriptions without asking your doctor. But caffeine? It’s everywhere. It’s in your coffee, your tea, your soda, your chocolate, your headache pills. And it’s powerful. It changes how your body handles medicine. If you take any prescription drug, talk to your pharmacist. Ask: “Does caffeine interfere with this?” Don’t assume it’s safe. The data is clear: when caffeine and meds collide, the consequences are real-and often preventable.



Albert Essel
December 2, 2025Caffeine's interaction with medications is one of those silent public health issues nobody talks about. I used to take my levothyroxine with my morning coffee-until my TSH jumped from 1.9 to 5.2. Turns out, 60 minutes isn’t just a suggestion; it’s a biological necessity. Now I take my pill at 6 AM, brush my teeth, and only drink coffee at 7. Simple. Free. Life-changing.
Charles Moore
December 3, 2025This is the kind of post that makes you pause. I never realized decaf could be an issue-thought it was just a harmless substitute. But if even 2-15 mg of caffeine can mess with thyroid meds, then maybe we all need to stop treating caffeine like it’s just a flavor. It’s a pharmacologically active compound. Treat it like one. Thanks for laying this out so clearly.
Gavin Boyne
December 5, 2025Oh wow, so caffeine is the silent drug dealer in my medicine cabinet? Thanks for the heads-up, Doc. I’ve been drinking 3 cups of coffee a day while on amitriptyline and wondering why I feel like a robot that got hit by a truck. Turns out, my liver’s been staging a coup. Guess I’m switching to herbal tea. Or maybe just napping. Either way, this post just saved me from a potential ER visit. And my therapist will thank you too.
Rashmin Patel
December 6, 2025OMG I’ve been doing this wrong for YEARS 😭 I take my Synthroid with my chai latte because ‘it helps me wake up’-and now I’m learning that my TSH has been floating because of it? I’m crying because I’m so mad at myself but also so grateful for this post. I just set a phone reminder: ‘PILL → 60 MIN → COFFEE’. I’m telling my entire family. This isn’t just health advice-it’s survival. Also, decaf isn’t safe?? My whole life is a lie. 🙃
sagar bhute
December 7, 2025This is just another fear-mongering article from people who don’t understand biology. Coffee is natural. Medications are synthetic. You’re telling me a plant compound is more dangerous than a lab-made chemical? Wake up. Most of these studies are observational. Correlation ≠ causation. Also, I’ve been drinking coffee with my meds for 12 years. I’m fine. You’re not.
Cindy Lopez
December 8, 2025So… coffee is bad with meds. Got it. I’ll just stop reading now.
James Kerr
December 9, 2025Whoa. I had no idea. I take warfarin and always thought my coffee was just my cozy morning ritual. Now I’m gonna stick to 1 cup, same time every day. And I’m telling my dad-he’s on 4 meds and drinks 4 coffees. He’s gonna hate me for this… but he’ll thank me later. 🤝☕
shalini vaishnav
December 10, 2025This is why Western medicine is so unreliable. In India, we’ve been drinking chai with Ayurvedic herbs for centuries without these ‘interactions’. You people overcomplicate everything. If your body can’t handle caffeine and pills together, maybe your body is weak. Or maybe you’re just addicted to Western pharmaceuticals. Chill. Drink your tea. Live.
vinoth kumar
December 12, 2025This is so useful. I’m on sertraline and never connected my anxiety spikes to my 2nd cup of coffee. I’m gonna cut back and track it for a week. Also, I never knew decaf had caffeine-now I get why my friend says she still feels jittery after switching. We need more posts like this. Thank you for sharing real, actionable info.
bobby chandra
December 12, 2025Let’s be real-caffeine is the original nootropic, the OG stimulant, the caffeine kingpin of the pharmacological universe. And now we’re learning it’s also the silent saboteur of your prescriptions? That’s wild. I used to think my heart racing after Adderall + coffee was just ‘productivity mode’. Turns out, it was my body screaming for mercy. I’m switching to water. And maybe a nap. And definitely a new life philosophy: if it’s in a cup, it’s a drug. Respect it.
Archie singh
December 13, 2025Interesting. But where’s the data on long-term outcomes? You cite studies but ignore confounding variables. Also, 127 drugs? That’s a number pulled from a hat. And why are you targeting coffee and not alcohol or sugar? Hypocrisy. You’re not educating-you’re scaring people into compliance.