
When treating pain in older adults, Mefenamic acid is a non‑steroidal anti‑inflammatory drug (NSAID) commonly prescribed for mild to moderate musculoskeletal pain and dysmenorrhea. It belongs to the anthranilic‑acid class of NSAIDs and works by inhibiting cyclooxygenase enzymes, reducing prostaglandin production. Because the elderly often have multiple health issues, understanding mefenamic acid safety is essential before adding it to a medication regimen.
Safety Concerns for Seniors
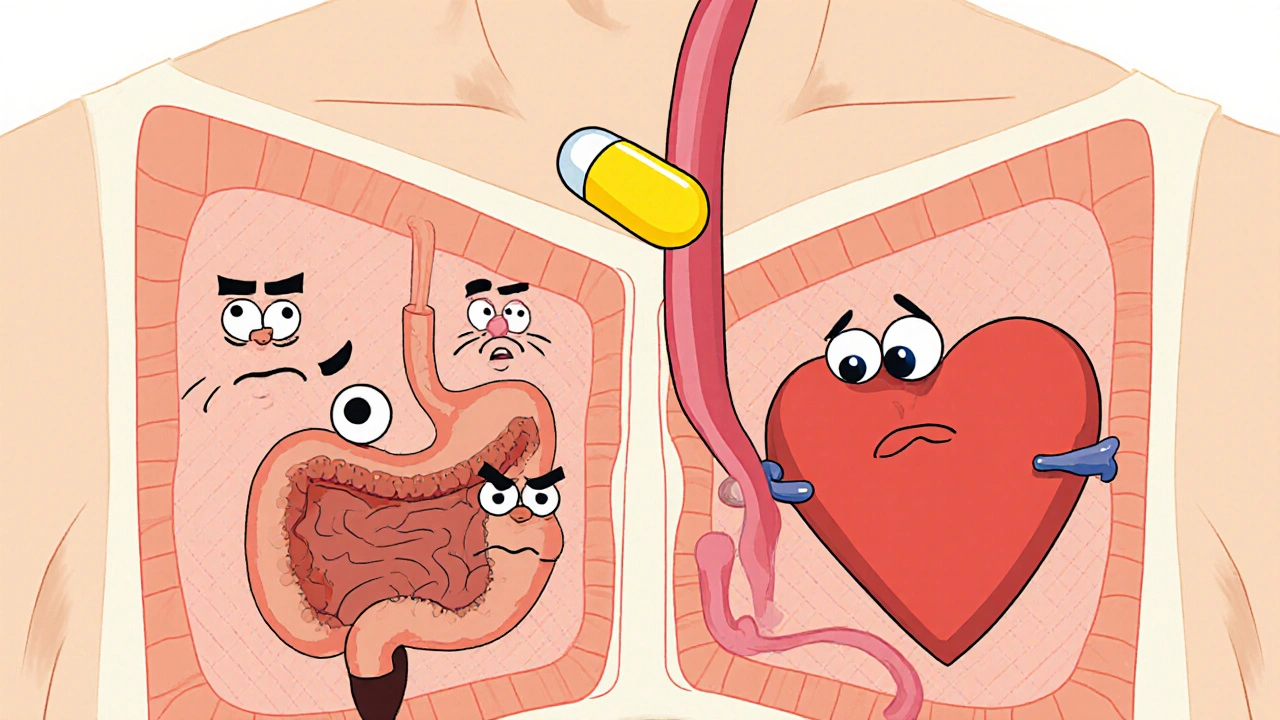
Older patients face a higher risk of gastrointestinal (GI) bleeding, renal impairment, and cardiovascular events when taking NSAIDs. Mefenamic acid is no exception. The drug can irritate the stomach lining, leading to ulcers or bleeding, especially in those with a history of peptic ulcer disease or who use anticoagulants. Renal function declines with age, and NSAIDs can further reduce blood flow to the kidneys, potentially precipitating acute kidney injury. Cardiovascular risk-such as increased blood pressure and heart‑failure exacerbation-must also be weighed.
Pharmacokinetics and Aging
Age‑related changes affect how the body absorbs, distributes, metabolizes, and excretes mefenamic acid. The drug’s half‑life (about 2 hours in young adults) can extend to 3‑4 hours in seniors due to slower hepatic metabolism and reduced renal clearance. Plasma protein binding may be altered by lower albumin levels, increasing the free drug fraction and the chance of side effects. These pharmacokinetic shifts mean that the same dose that’s safe for a 35‑year‑old could be excessive for an 80‑year‑old.
Recommended Dosage in Elderly Patients
Guidelines suggest a lower initial dose and a shorter treatment duration for older adults:
- Initial dose: 250 mg orally every 6 hours.
- Maximum daily dose: 750 mg (i.e., three 250 mg doses) for a maximum of 5 days.
- If pain persists, consider alternating with acetaminophen rather than increasing the dose.
For patients with mild to moderate renal impairment (creatinine clearance 30‑50 mL/min), the dose should be reduced to 125 mg every 8 hours, not exceeding 375 mg per day. Those with severe renal failure should avoid mefenamic acid altogether.
Contraindications & When to Avoid
Mefenamic acid should be withheld in the following situations:
- Known hypersensitivity to anthranilic‑acid NSAIDs.
- Active or recent (< 3 months) GI ulcer or bleeding.
- Severe heart failure (NYHA class III‑IV) or uncontrolled hypertension.
- Advanced chronic kidney disease (eGFR < 30 mL/min/1.73 m²).
- Concurrent use of anticoagulants such as warfarin without close INR monitoring.
Pregnant women (especially in the third trimester) and patients with asthma exacerbated by NSAIDs should also avoid it.
Managing Common Side Effects
When side effects arise, a step‑wise approach can help:
- Stomach upset: Take the medication with food or a full glass of milk; consider a proton‑pump inhibitor (omeprazole 20 mg daily) for protection.
- Headache or dizziness: Verify hydration status and assess for hypotension.
- Kidney‑related symptoms: Monitor serum creatinine and urine output; discontinue if creatinine rises > 0.3 mg/dL within 48 hours.
Educate patients and caregivers to report any new bruising, dark stools, or sudden swelling promptly.
Drug Interactions Important for Older Adults
Polypharmacy is common in seniors, making interaction checks vital. Notable interactions include:
- Anticoagulants (warfarin, dabigatran): Heightened bleeding risk; monitor INR or thrombin time.
- Other NSAIDs (ibuprofen, naproxen): Additive GI and renal toxicity; avoid concurrent use.
- ACE inhibitors or ARBs: Reduced renal perfusion; monitor blood pressure and kidney function.
- Selective serotonin reuptake inhibitors (SSRIs): Increased bleeding risk.
- Diuretics: Potential for electrolyte imbalance and worsening renal function.
Always review the full medication list before prescribing.
Comparison with Other NSAIDs Commonly Used in Seniors
| NSAID | Typical Dose (Elderly) | Half‑Life | GI Risk | Renal Risk | Cardiovascular Risk |
|---|---|---|---|---|---|
| Mefenamic acid | 250 mg q6h (max 750 mg/day) | 2‑4 h | Moderate | Moderate | Low‑moderate |
| Ibuprofen | 200‑400 mg q6‑8h (max 1200 mg/day) | 2‑4 h | Moderate | Low‑moderate | Low‑moderate |
| Naproxen | 250 mg q12h (max 500 mg/day) | 12‑17 h | Low | Low | Low |
| Diclofenac | 50 mg q12h (max 100 mg/day) | 1‑2 h | High | High | High |
From the table, naproxen shows the lowest GI and renal risk, while diclofenac carries the highest cardiovascular danger. Mefenamic acid sits in the middle, making it a reasonable option when short‑term use is needed and other agents are unsuitable.
Practical Recommendations for Clinicians & Caregivers
To use mefenamic acid safely in older adults, follow these steps:
- Conduct a thorough medication review, focusing on anticoagulants, other NSAIDs, and antihypertensives.
- Assess baseline renal function (eGFR) and GI history.
- Start with the lowest effective dose (250 mg q6h) and limit therapy to 5 days.
- Prescribe gastro‑protective agents if the patient has a prior ulcer or is on low‑dose aspirin.
- Schedule follow‑up labs (creatinine, electrolytes) after 48‑72 hours, especially if the patient has comorbid kidney disease.
- Educate the patient and caregiver on warning signs: black stools, sudden swelling, or dizziness.
- If pain persists beyond 5 days, switch to acetaminophen or consider physical therapy before restarting NSAIDs.
Documenting these measures in the medical record helps ensure continuity of care across providers.
Frequently Asked Questions
Can an elderly patient take mefenamic acid with aspirin?
Low‑dose aspirin combined with mefenamic acid significantly raises the risk of GI bleeding. If aspirin is essential for cardiovascular protection, a gastro‑protective agent (e.g., a proton‑pump inhibitor) should be added, and the NSAID dose kept at the minimum effective level.
How often should kidney function be checked while on mefenamic acid?
For seniors with borderline renal function, check serum creatinine and eGFR before starting therapy and repeat the test after 48‑72 hours. If there is a rise of ≥ 0.3 mg/dL, discontinue the drug.
Is mefenamic acid safe for patients on warfarin?
Mefenamic acid can potentiate warfarin’s anticoagulant effect, leading to a higher INR. If co‑prescription is unavoidable, monitor INR closely (every 2‑3 days) and adjust warfarin dose as needed.
What are alternatives to mefenamic acid for elderly patients?
Acetaminophen is first‑line for mild‑to‑moderate pain with a better safety profile. If an NSAID is required, naproxen or low‑dose ibuprofen (with gastro‑protection) are preferred due to lower renal and cardiovascular risks.
How long can a senior safely stay on mefenamic acid?
The drug is intended for short‑term use only-generally no more than 5 days. Prolonged therapy significantly raises the chance of ulceration, kidney injury, and hypertension.



Greg Galivan
October 25, 2025Look, the 250 mg q6h starter isn’t a suggestion-it’s a hard limit for seniors. If you bump it to 500 mg you’re begging for GI bleeds and kidney trouble. The pharmacokinetics shift in the elderly means the drug sticks around longer, so the “standard” adult dose just ain’t safe here.
Anurag Ranjan
October 26, 2025Make sure to check kidney labs before and after starting, and add a PPI if the patient has any ulcer hx.
James Doyle
November 1, 2025The pharmacodynamic profile of mefenamic acid, particularly its cyclooxygenase inhibition kinetics, necessitates a vigilant risk‑benefit assessment in geriatric cohorts.
While the drug’s half‑life extends modestly in older adults, the resultant increase in free plasma concentration can precipitate disproportionate prostaglandin suppression.
This suppression, in turn, compromises gastric mucosal integrity, elevating ulcerogenic potential beyond the baseline risk associated with age alone.
Renal hemodynamics are likewise vulnerable; NSAID‑induced afferent arteriole constriction reduces glomerular filtration, making acute kidney injury a plausible sequela in patients with pre‑existing nephropathy.
Cardiovascular homeostasis is not exempt, as NSAIDs may attenuate the efficacy of antihypertensive agents through sodium retention and vasoconstrictive mechanisms.
Therefore, when prescribing mefenamic acid to seniors, one must integrate a multi‑parameter monitoring framework: baseline eGFR, periodic serum creatinine, and vigilant surveillance for occult gastrointestinal bleeding.
Concomitant use with anticoagulants amplifies hemorrhagic risk, necessitating either dose adjustment or prophylactic gastro‑protective therapy.
In clinical practice, a step‑wise algorithm that initiates therapy at 250 mg q6h, caps the duration at five days, and mandates reassessment at 48‑hour intervals aligns with best‑practice guidelines.
Should analgesic efficacy prove insufficient, transitioning to acetaminophen or non‑pharmacologic modalities such as physical therapy is advisable before escalating NSAID exposure.
It is also prudent to educate patients and caregivers about cardinal warning signs-melena, hematemesis, abrupt edema, or unexplained dizziness-and to provide clear directives for immediate medical evaluation.
From a formulary perspective, alternative NSAIDs with more favorable renal and gastrointestinal safety profiles, such as naproxen, may be preferential in polypharmacy contexts.
Nevertheless, mefenamic acid retains a niche role for short‑term, breakthrough pain when other agents are contraindicated or ineffective.
In summary, the therapeutic window for mefenamic acid in the elderly is narrow, demanding judicious dosing, rigorous monitoring, and a low threshold for discontinuation at the first sign of adverse events.
Edward Brown
November 2, 2025What most don’t tell you is that the pharma push for NSAIDs like mefenamic is tied to hidden incentives. They downplay the renal risks while marketing the “short‑term” label as harmless. It’s no coincidence that the same companies sponsor continuing‑education courses that stress pain relief over safety. The data they highlight often omit elderly sub‑analyses, leaving us with an incomplete picture. So, when you see a guideline that seems too convenient, ask who benefited from it.
ALBERT HENDERSHOT JR.
November 3, 2025While it’s prudent to be cautious, the evidence does support limited short‑term use when alternatives fail. Adding a gastro‑protective agent and close INR monitoring can mitigate many of the concerns you highlighted 😊.
Suzanne Carawan
November 13, 2025Oh joy, another “must‑read” guide on mefenamic acid for the elderly-just what we all were missing in the pharmacy aisle.
Kala Rani
November 14, 2025Actually the dosage limits are just marketing fluff.
Donal Hinely
November 15, 2025Don’t be a snob, the guidelines are there for a reason-skip the drama and stick to the science, or you’ll end up with a patient bleeding on the floor.
christine badilla
November 16, 2025Can you imagine the horror of a senior collapsing in the hallway because someone ignored a simple dose cap? The tragedy is real, and it haunts every caregiver’s night.
Octavia Clahar
November 17, 2025We’ve all seen those scary moments, but with vigilant monitoring and a bit of kindness, we can keep our patients safe and comfortable.
eko lennon
November 18, 2025When I was on my first rotation, I saw a 78‑year‑old on mefenamic acid without any renal checks. Within two days his creatinine spiked, and the team scrambled to stop the drug. It was a wake‑up call about how easy it is to overlook the “short‑term” label. The lesson? Always pair the NSAID with a renal baseline and a clear stop‑date. Even a single missed lab can turn a manageable pain regimen into a crisis. So, keep the dosing low, watch the labs, and never assume the patient is fine just because they “feel better”.