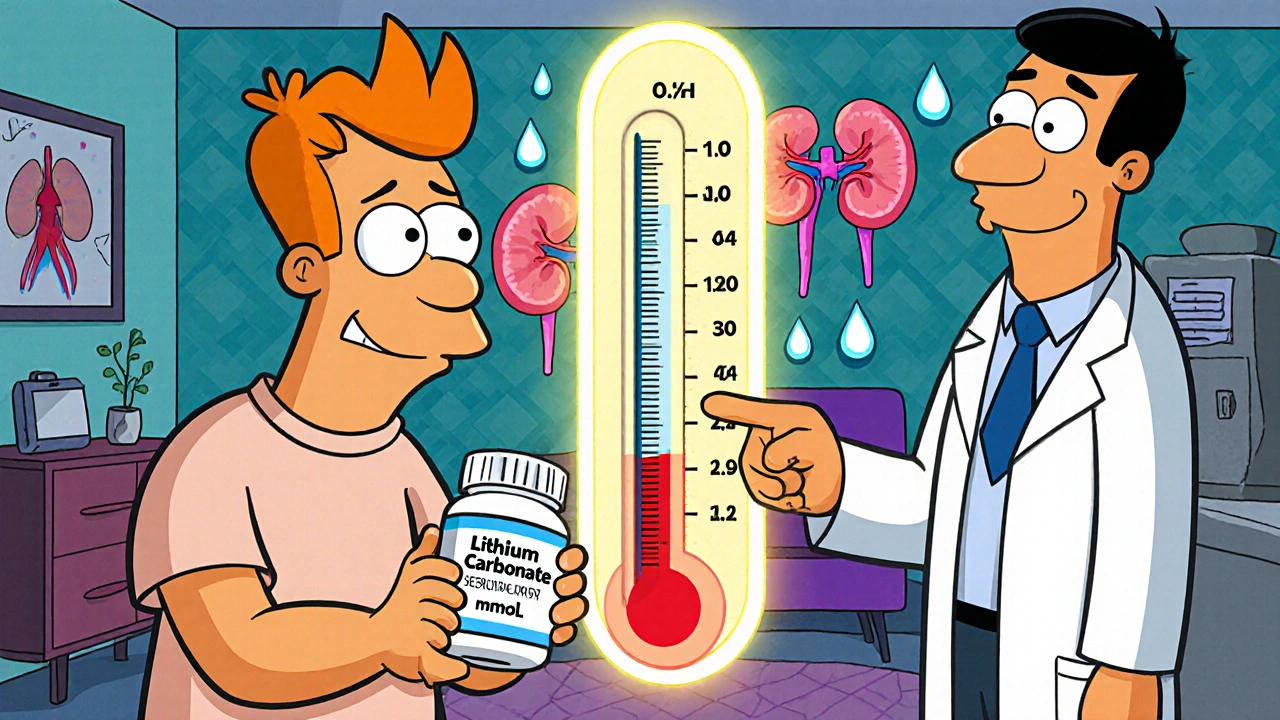
Lithium Therapeutic Range: What You Need to Know About Dosage and Safety
When doctors prescribe lithium, a mood stabilizer used primarily for bipolar disorder. Also known as lithium carbonate, it helps prevent extreme mood swings—but only if your blood levels stay in the right zone. This zone, called the lithium therapeutic range, is narrow: usually between 0.6 and 1.2 milliequivalents per liter (mEq/L). Go below that, and the drug might not control your mania or depression. Go above it, and you risk serious side effects like tremors, confusion, or even kidney damage.
That’s why regular blood tests aren’t optional—they’re life-saving. Your body doesn’t process lithium the same way everyone else does. Age, kidney function, salt intake, and even dehydration can shift your levels overnight. Someone on 600 mg daily might be perfectly safe, while another person on the same dose could be heading toward toxicity. That’s not a guess—it’s science. Studies show that over 50% of lithium-related hospital visits happen because levels weren’t monitored closely enough. And if you’re also taking diuretics, NSAIDs, or ACE inhibitors, your risk goes up even more. These drugs interfere with how your kidneys clear lithium, so even small changes in your routine can have big consequences.
It’s not just about the number on the lab report. How you feel matters too. Mild nausea, frequent urination, or a slight hand shake might seem like minor annoyances—but they’re early warnings. If you start feeling dizzy, slurring your words, or losing coordination, that’s not normal. It’s your body screaming that your lithium level is too high. And if you’re on lithium for bipolar disorder, you know how fragile stability can be. One bad week of sleep, a sudden illness, or skipping a dose can throw everything off. That’s why your doctor needs to see you often, especially when you first start or if your dose changes.
There’s no one-size-fits-all target. Some people feel best at 0.6, others need 1.0. It depends on your symptoms, your metabolism, and how your brain responds. But the goal is always the same: keep you stable without putting you at risk. That’s why lithium isn’t just a pill—it’s a partnership between you, your doctor, and consistent testing. You can’t manage it on your own. You need the numbers, the symptoms, and the timing all working together.
Below, you’ll find real stories and practical advice from people who’ve walked this path. From how to handle side effects to why some generics don’t work the same as others, these posts give you the tools to stay safe and in control. Whether you’re just starting lithium or have been on it for years, there’s something here that could make a difference.