Drug Formulary: What It Is and How It Affects Your Medication Choices
When your doctor prescribes a medication, the first question isn’t always whether it works—it’s whether your drug formulary, a list of approved medications covered by your health plan. Also known as a preferred drug list, it determines what you can get, at what price, and sometimes whether you need prior approval just to fill the prescription. This isn’t just paperwork—it’s the hidden gatekeeper between you and the medicine your body needs.
Every insurance plan, from Medicare Part D to private employer plans, uses a drug formulary, a curated list of medications deemed safe, effective, and cost-efficient by a pharmacy and therapeutics committee. These lists aren’t random. They’re built using clinical evidence, cost data, and sometimes negotiations with drug makers. That’s why two people with the same condition might get different prescriptions: one’s plan covers the brand-name drug, another’s only covers the generic. And if your drug isn’t on the list? You might pay full price, get denied, or be forced to try cheaper alternatives first—what’s called step therapy, a process where insurers require you to try lower-cost drugs before approving more expensive ones.
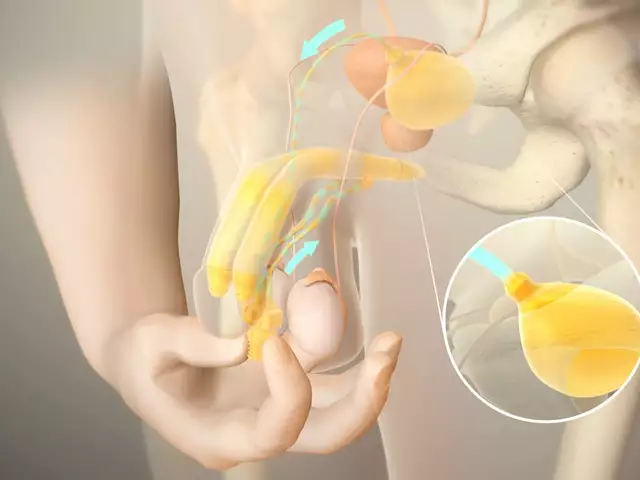
It’s not just about cost. Formularies also control access based on risk. For example, drugs like simvastatin 80 mg or omeprazole with clopidogrel might be restricted because of known interactions. Others, like nitrofurantoin, come with warnings for people with G6PD deficiency. Your plan’s formulary might block these unless you prove you’ve been tested or have no safer options. Even common OTC meds like acetaminophen or decongestants can be affected if they’re part of combo products that insurers don’t want to encourage.
But here’s the thing: formularies change. New drugs get added, old ones get pulled, and coverage rules shift every year. Medicare Part D formularies update annually, and private plans follow suit. That’s why you might fill a prescription one year, only to be told the next year it’s no longer covered. The same goes for copay assistance programs—many only work with formulary-approved drugs. If your medication isn’t on the list, even a discount coupon might not help.
What you’ll find in this collection are real-world guides on how to navigate these systems. From how to challenge a formulary denial, to understanding why certain drugs like mefenamic acid or Accufine are treated differently, to how governments keep generic prices low without price caps—you’ll see how the rules actually play out for patients. You’ll learn how to read your plan’s formulary, when to ask for an exception, and which drugs are most likely to be restricted based on real data from FDA labels, drug interactions, and patient cost barriers. This isn’t theory. It’s what happens when insurance rules meet your medicine cabinet.