Conjugated Estrogens: What They Are and How They Work
If you’ve ever heard a doctor mention "conjugated estrogens" and felt lost, you’re not alone. These are a mix of estrogen hormones taken from natural sources, usually horse urine, and they mimic the estrogen your body makes. When you take them, they bind to estrogen receptors, helping balance hormone levels that may be low during menopause or after certain surgeries.
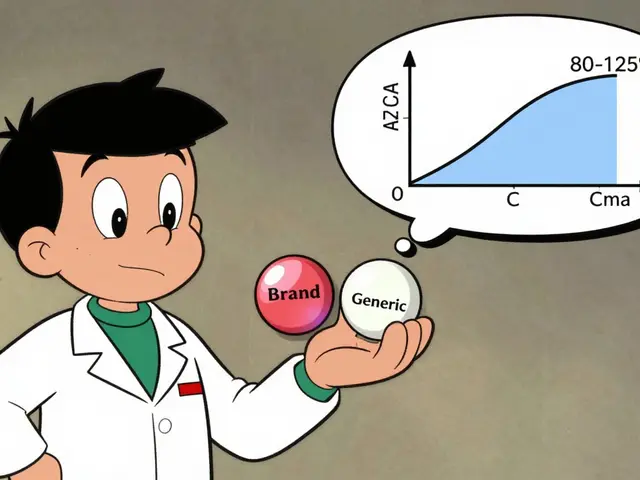
The most common brand you’ll see is Premarin, but many generic versions exist. They come in tablet, patch, or cream form, giving you flexibility based on your lifestyle and how your skin reacts. The goal is simple: reduce hot flashes, protect bone density, and improve mood without overloading your system.
When Doctors Prescribe Conjugated Estrogens
Doctors usually turn to conjugated estrogens for women experiencing moderate to severe menopause symptoms, especially if they haven’t found relief with lifestyle changes alone. They also use them after oophorectomy (removal of ovaries) to replace the estrogen the ovaries would have made. In some cases, they pair the estrogen with a progesterone‑like drug to protect the uterus from lining overgrowth.
Typical starting doses are low – often 0.3 mg to 0.45 mg per day for tablets – and the doctor will adjust based on your symptom relief and any side effects. If you’re on a patch, you might start with a patch delivering 0.025 mg per day. The key is to start low and move up only if needed.
Key Benefits, Common Side Effects, and Safety Tips
Most users notice a drop in hot flashes within a few weeks. You may also feel better sleep, smoother skin, and fewer mood swings. Bone health gets a boost, too, because estrogen helps keep calcium in your bones.
Side effects aren’t rare. Some people get breast tenderness, mild nausea, or spotting between periods. More serious, but less common, issues include blood clots, high blood pressure, or gallbladder problems. If you notice sudden leg pain, shortness of breath, or severe headaches, call your doctor right away.
Safety tips are straightforward: keep regular check‑ups, track any new symptoms, and never add another hormone product without medical advice. If you have a history of blood clots, heart disease, or hormone‑sensitive cancers, discuss alternatives first.
Speaking of alternatives, many women now try bioidentical hormone therapy, which uses plant‑derived hormones that match your body’s own estrogen. Lifestyle tweaks like a plant‑rich diet, regular exercise, and stress management can also lower hot flashes without medication.
In short, conjugated estrogens can be a useful tool for managing menopause symptoms, but they work best when paired with a solid plan that includes doctor monitoring and healthy habits. Talk to your healthcare provider to see if they’re right for you, and remember that the lowest effective dose is usually the safest choice.