Brain Surgery: Risks, Recovery, and What You Need to Know
When someone talks about brain surgery, a medical procedure to treat conditions inside the skull, often performed by a neurosurgeon. Also known as neurosurgery, it's not something you hear about every day—but when it happens, it changes everything. Whether it's removing a tumor, relieving pressure after a stroke, or fixing a blood vessel, brain surgery is precise, high-stakes, and deeply personal.
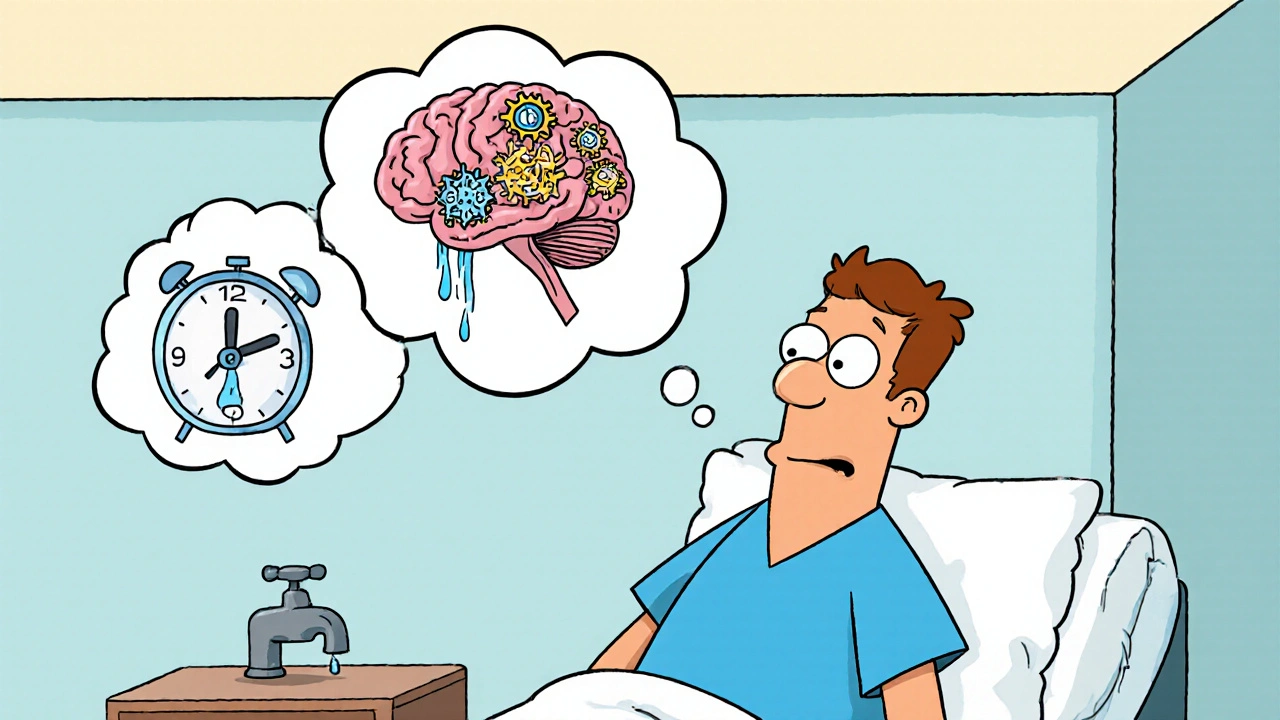
It’s not just about the operation itself. The real challenge often comes after—recovering from brain surgery means relearning simple things like walking, talking, or remembering names. Many people don’t realize how much recovery depends on the area of the brain affected. A tumor near the speech center? That can mean weeks of speech therapy. A bleed in the motor cortex? Physical rehab becomes the new daily job. And it’s not just the patient. Families often become full-time caregivers, learning how to manage seizures, mood swings, or memory lapses that show up weeks after the surgery.
Not every brain issue needs surgery. Sometimes medication, radiation, or monitoring is enough. But when surgery is the best—or only—option, knowing what to expect cuts through the fear. You need to understand the risks: infection, bleeding, or even permanent changes in personality or function. But you also need to know the success rates. For example, removing a benign meningioma has a high success rate with low long-term side effects. Removing a deep-seated glioblastoma? That’s a different story, with survival measured in months, not years. The type of surgery matters too. Craniotomy? Minimally invasive endoscopic? Stereotactic radiosurgery? Each has its own recovery timeline and risks.
And let’s be real—brain surgery doesn’t happen in a vacuum. It’s tied to other health issues. High blood pressure can increase bleeding risk. Diabetes slows healing. Medications like blood thinners might need to be stopped days before. Even something as simple as smoking can mess with oxygen flow to the brain during recovery. That’s why doctors spend so much time prepping you—not just for the knife, but for the weeks and months after.
There’s no one-size-fits-all guide to brain surgery recovery. But what you’ll find below are real, practical posts from people who’ve been through it—or helped someone who has. You’ll read about the hidden dangers of post-op infections, how to spot early signs of complications, what medications to watch out for during recovery, and why some patients bounce back faster than others. You’ll see how brain surgery connects to other conditions like epilepsy, stroke, or even chronic headaches. And you’ll find out which treatments are backed by real data—not just hype.