
When your prescription runs out and the pharmacy says it’s backordered-again-you’re not alone. In 2025, over 350 drugs in the U.S. were in short supply, from simple antibiotics to life-saving cancer treatments. For many, the answer isn’t waiting or switching brands. It’s compounding pharmacies.
What Exactly Is a Compounding Pharmacy?
A compounding pharmacy doesn’t just fill prescriptions. It builds them. These labs take raw chemical ingredients and mix them into custom formulations that aren’t made by big drug companies. Need a medicine without dyes because you’re allergic? Done. Need a liquid version because swallowing pills is impossible? Easy. Need a lower dose than what’s commercially available? They’ll make it. Unlike regular pharmacies that stock pre-made pills, compounding pharmacies are like medical kitchens. They work with pharmacists trained in chemistry and dosage precision. They follow strict standards like USP <795> for non-sterile mixes and USP <797> for sterile ones-think clean rooms, calibrated scales, and quality checks that most retail pharmacies don’t have.Why Do People Turn to Them?
It’s not just about shortages. It’s about fit. About 1 in 5 people have sensitivities to common fillers like lactose, gluten, or artificial colors in commercial drugs. For them, even a tiny amount can cause rashes, stomach pain, or worse. Compounding pharmacies remove those triggers. A patient with chronic migraines might get a topical gel instead of an oral pill that makes them nauseous. A child with epilepsy might get a strawberry-flavored liquid that they’ll actually take. Pediatric and geriatric patients benefit the most. Around 40% of kids can’t swallow pills. About 30% of seniors have trouble swallowing too. Compounding turns tablets into drops, creams, or even lollipops. One parent in Melbourne told me her 6-year-old hadn’t taken her ADHD meds in months-until the pharmacist made a bubblegum-flavored suspension. Adherence jumped from 20% to 90%.When Drug Shortages Hit
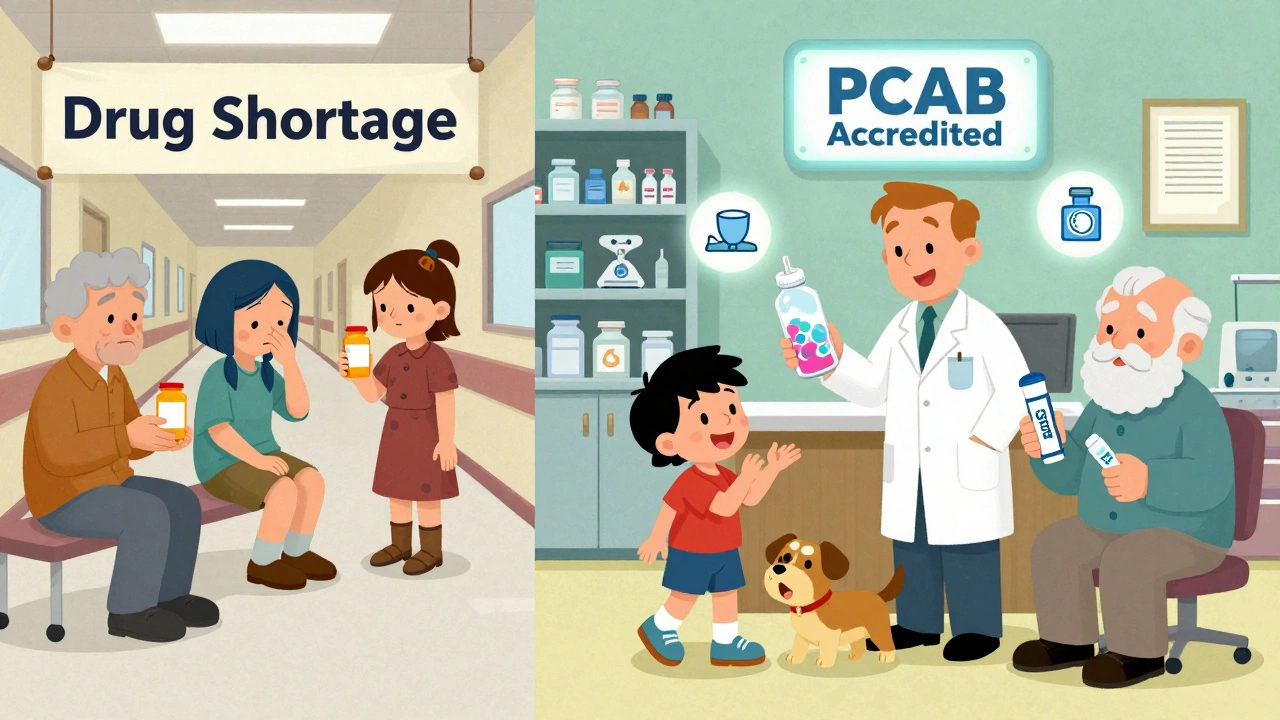
In 2023, the FDA recorded 387 drug shortages. Some were temporary. Others lasted over a year. Think of thyroid meds, injectable antibiotics, or even basic painkillers like morphine. When these disappear, hospitals and clinics scramble. That’s where compounding pharmacies step in. They can replicate many of these drugs-like methylphenidate or hydrocortisone-using the same active ingredients. A 2023 study found that when a commercial version of a drug was unavailable, 85% of patients on compounded versions stayed on their treatment plan. Without compounding, many would’ve gone without. But there’s a limit. Compounding pharmacies can’t make biologics-like insulin or monoclonal antibodies. These require complex biological processes only big manufacturers can handle. They also can’t copy brand-new drugs that haven’t been approved yet. Compounding is a bridge, not a replacement.
How It Works: From Doctor to Doorstep
It starts with your doctor. They don’t just write a script for a compounded med-they have to explain why the commercial version won’t work. That could be an allergy, a swallowing issue, or a shortage. Then they send a detailed prescription to a compounding pharmacy. The pharmacist reviews it, checks ingredient availability, and confirms the formula is safe and stable. Most compounded meds take 24 to 72 hours to prepare. Sterile ones-like injections or IV solutions-take longer because they need extra testing. You’ll usually pay out of pocket. Insurance rarely covers compounded drugs unless it’s a rare case. About 45% of patients pay full price, compared to just 15% for regular prescriptions. But many say it’s worth it. One survey found 89% of patients who used compounded meds would recommend them to others with similar needs.What to Look for in a Compounding Pharmacy
Not all compounding pharmacies are equal. Some are small, local labs with strict protocols. Others cut corners. The best ones are accredited by the Pharmacy Compounding Accreditation Board (PCAB). There are only about 1,200 PCAB-accredited pharmacies in the U.S.-out of 7,500 that do compounding. Ask if they:- Have a clean room with air filtration
- Test each batch for potency and purity
- Provide a certificate of analysis with your medication
- Work directly with your doctor to adjust doses
Real Cases That Made a Difference
A man in Arizona with severe eczema couldn’t use steroid creams because they contained preservatives that burned his skin. His dermatologist teamed up with a compounding pharmacy to make a preservative-free version. Within weeks, his flare-ups dropped by 80%. A woman with chronic pain needed a lower dose of gabapentin than what’s sold. The standard tablet was 100mg, but she reacted to anything over 25mg. Her pharmacist made capsules with exactly 25mg, using a powder form that didn’t contain fillers she was allergic to. She went from bedridden to walking her dog daily. Even in mental health, compounding helps. One Reddit user shared how switching from oral finasteride (which caused sexual side effects in 32% of users) to a topical compounded version reduced side effects to just 8%.Limitations and Risks
Compounding isn’t magic. It’s medicine-with trade-offs. First, no pre-market testing. FDA-approved drugs go through years of trials. Compounded meds don’t. That’s why experts warn: don’t use them if a commercial version is available and safe. Second, consistency can vary. If a pharmacy doesn’t follow strict protocols, your dose might be too high or too low. That’s why accreditation matters. Third, wait times. You can’t walk in and get it today. If you’re in urgent need, it won’t help. But if you’ve got a few days, it’s often the only option.Is This the Future of Medicine?
More people are asking for personalized care. Genetic testing is becoming common. Pharmacists are starting to tailor meds based on how someone metabolizes drugs. Compounding pharmacies are at the front of that shift. The market is growing fast. It was worth $11.2 billion in 2022 and is projected to hit $15.8 billion by 2027. That’s because shortages aren’t going away. Drug manufacturing is fragile. Supply chains break. And patients are tired of being stuck. Compounding pharmacies aren’t the answer to every problem. But for the people who can’t take the pills on the shelf-they’re essential.Are compounded medications safe?
Yes, when made by an accredited pharmacy that follows USP guidelines. Compounded meds don’t go through FDA approval like mass-produced drugs, but they’re held to strict quality standards. Always choose a PCAB-accredited pharmacy and ask for batch testing results.
Can any pharmacy compound medications?
No. While about 32,000 U.S. pharmacies offer some compounding, only 7,500 specialize in it. Most retail pharmacies lack the equipment, training, or clean rooms needed. Always confirm the pharmacy is set up for compounding-not just filling scripts.
Does insurance cover compounded prescriptions?
Usually not. About 45% of patients pay out of pocket. Some insurers will cover it if your doctor proves the commercial version won’t work-for example, due to allergies or dosage issues. Always check with your insurer before starting.
How long does it take to get a compounded medication?
Typically 24 to 72 hours. Simple non-sterile mixes (like creams or liquids) can be ready in a day. Sterile compounds, like injections, may take longer because they require extra testing for safety. Plan ahead-don’t wait until your last pill is gone.
Can compounding pharmacies make any drug?
No. They can’t replicate complex biologics like insulin, vaccines, or monoclonal antibodies. They also can’t make drugs that require FDA-approved manufacturing processes. Compounding is for when standard drugs aren’t suitable-not when they’re simply unavailable.

Iris Carmen
December 9, 2025so i just found out my kid’s ADHD med was compounded and i thought it was some fancy new drug lmao
Sarah Gray
December 10, 2025Let’s be clear: compounding pharmacies are not a ‘solution’-they’re a symptom of a broken pharmaceutical supply chain. The fact that we’ve normalized patching systemic failures with artisanal meds is less ‘innovation’ and more ‘desperation dressed in lab coats.’ USP standards? Fine. But without federal oversight, you’re gambling with bioequivalence. And don’t get me started on the 45% paying out-of-pocket-this is healthcare inequity dressed as customization.
Shubham Mathur
December 12, 2025People dont realize how many lives this saves my cousin in India cant get his epilepsy med because of import bans so his doctor sent a script to a compounding lab in Texas and now he takes a strawberry liquid every night and sleeps without seizures for the first time in 7 years i mean come on this isnt magic its basic human care
Stacy Tolbert
December 12, 2025I’ve been on compounded thyroid meds for 11 years. I had to stop the commercial ones because they gave me hives and panic attacks. My pharmacist literally called my doctor to tweak the dose. I cried the first time I took it and didn’t feel like I was going to die. This isn’t a luxury. It’s survival. And yes, I pay full price. I’d pay double.
Ronald Ezamaru
December 13, 2025Compounding pharmacies are one of the most underappreciated pillars of patient-centered care in the U.S. They bridge gaps that big pharma ignores-pediatric dosing, allergen-free formulations, even flavor customization for elderly patients with dysphagia. The real issue isn’t the practice-it’s the lack of standardized reimbursement and inconsistent accreditation enforcement. PCAB accreditation should be mandatory, not optional. And insurance companies need to stop treating these as ‘experimental’ when they’re clinically essential for thousands.
Delaine Kiara
December 14, 2025Okay but let’s talk about the fact that some of these pharmacies are literally making lollipops for kids who won’t swallow pills?? I mean, who even thought of that?? And then there are the ones selling ‘miracle’ hormone creams online that smell like lavender and cost $200 a tube-NO. Just no. Compounding is lifesaving when done right, but the internet turned it into a wellness cult with a pharmacy license. Also, why is it still so hard to find a PCAB-accredited one? I searched for 3 weeks. 3 WEEKS. And the ones that are accredited? They’re in New York, Chicago, and LA. Good luck in rural Kansas.
Ruth Witte
December 14, 2025THIS IS THE FUTURE!!! 🚀💖 I used to cry every time I had to take my gabapentin because the fillers made me feel like I was being stabbed in the throat. Now I take a tiny gel cap with no junk in it and I can actually walk my dog again!! I LOVE MY COMPOUNDING PHARMACY!! THEY’RE ANGELS IN WHITE COATS!! 🌈💊✨
Noah Raines
December 16, 2025My dad’s on a compounded version of his blood pressure med because he’s allergic to the dye. Took 4 months to get it approved by insurance but now he’s not dizzy all day. Honestly, if you’ve got a legit medical reason, it’s worth the hassle. Just don’t go ordering stuff off some shady website. And yeah, it’s expensive-but so is ER visits from bad reactions.
Katherine Rodgers
December 17, 2025Oh wow, so now we’re romanticizing pharmacies that operate in a regulatory gray zone? Congrats, you’ve turned a workaround into a lifestyle brand. ‘My compounding pharmacist is my soulmate.’ Really? Because the FDA didn’t test it. And no, ‘batch testing’ doesn’t replace phase 3 trials. Also, 89% would recommend it? Yeah, because they’re desperate. Not because it’s better. Just sayin’.
Lauren Dare
December 19, 2025Let’s deconstruct the rhetoric: ‘personalized medicine’ is just a euphemism for ‘we can’t standardize this so we’re outsourcing risk to pharmacists.’ The fact that you need a doctor to justify why you can’t take the FDA-approved version is a failure of drug design, not a triumph of compounding. And don’t get me started on the ‘certificate of analysis’-that’s not a guarantee, it’s a receipt. Quality control is only as good as the lab’s SOPs, and most aren’t audited. This isn’t innovation. It’s triage.
Gilbert Lacasandile
December 21, 2025I’ve worked in a compounding pharmacy for 8 years. We make everything from hormone creams to pediatric antibiotics. We test every batch. We work with doctors. We don’t advertise online. We don’t sell bulk. And we’re one of the few in our state that’s PCAB-accredited. It’s not glamorous. It’s not profitable. But it’s necessary. I wish more people knew how hard we work to get this right.
Taya Rtichsheva
December 22, 2025my cousin got her migraine med compounded into a nasal spray and now she doesnt need to nap for 6 hours after work i mean who even thought of that
Christian Landry
December 24, 2025my grandma got her pain med turned into a lollipop and she says it tastes like candy and she takes it every day now 😊 she used to just lie on the couch crying. this stuff matters man