More than 1 in 10 adults over 80 in the U.S. are taking prescription sleep meds every month. That’s not just a number-it’s a reality for millions who wake up hoping tonight will be different. But what happens when the pill that helps you fall asleep starts stealing your safety, your memory, and your ability to quit?
The Hidden Cost of a Good Night’s Sleep
Sleep medications don’t fix insomnia. They mask it. And like any quick fix, the bill comes later. Benzodiazepines like lorazepam and non-benzodiazepine Z-drugs like zolpidem (Ambien) and eszopiclone (Lunesta) work by slowing down your brain. They’re not sleep enhancers-they’re CNS depressants. That means they don’t just help you fall asleep. They change how your brain cycles through sleep stages, often reducing deep, restorative sleep while increasing light, fragile stages.That’s why so many people wake up feeling foggy. About 25% of users report next-day drowsiness, impaired coordination, or memory lapses. In older adults, that’s not just annoying-it’s dangerous. The American Geriatrics Society says these drugs increase fall risk by 50-60% and fracture risk by 20-30%. A single stumble can mean a broken hip, months in rehab, or worse. And yet, these meds are still prescribed to seniors far too often.
The FDA has issued multiple warnings. In 2019, it cut the recommended starting dose of zolpidem for women from 10mg to 5mg after evidence showed residual impairment equivalent to a blood alcohol level of 0.05-0.08%. That’s legally drunk in many states. People have driven while still under the drug’s influence. Others have cooked, eaten, or even had conversations-then had no memory of it the next morning. These aren’t rare side effects. They’re documented, FDA-recognized risks.
Dependence Isn’t Just a Word-It’s a Trap
You don’t need to be a drug addict to become dependent on sleep meds. Dependence happens when your body adapts. You need the same dose to get the same effect. Then you need more. Then you panic when you run out. And when you stop? Rebound insomnia hits hard.Studies show up to 33% of people using benzodiazepines regularly for more than four weeks develop dependence. Z-drugs are a bit lower-around 5-10%-but that still means tens of thousands of people each year get stuck. One Reddit user wrote: “After six months of nightly Ambien, I tried to quit. Couldn’t sleep for three nights straight. Ended up back on it.” That’s not weakness. That’s pharmacology.
Doctors often don’t warn patients about this. They hand out a 30-day script and assume you’ll stop when it’s gone. But the body doesn’t work that way. Discontinuing these drugs isn’t like stopping a vitamin. It requires a slow taper-usually 25% every two weeks. And even then, 40% of people need extra support to get through withdrawal. Anxiety, racing heart, nightmares, and insomnia worse than before can last for weeks. That’s why so many people stay on them longer than intended. They’re not addicted to the drug. They’re addicted to the idea of sleeping without it.
Over-the-Counter Sleep Aids: A False Sense of Safety
Diphenhydramine (Benadryl) and doxylamine (Unisom) are everywhere. Cheap. Easy to buy. No prescription needed. But they’re not harmless. These are anticholinergic drugs-same class as some older Alzheimer’s medications. A 2015 JAMA Internal Medicine study found that long-term use of these OTC sleep aids increased dementia risk by 54%.They also cause dry mouth, blurred vision, constipation, and urinary retention. In older adults, these effects can mimic dementia or worsen existing conditions. And they don’t work well long-term. The body builds tolerance fast. What helped you fall asleep last month might do nothing this month. Yet people keep taking them, thinking, “It’s just an antihistamine.” It’s not just an antihistamine. It’s a brain-altering drug with serious long-term consequences.
Melatonin is another popular choice. It’s not a sedative. It’s a hormone that signals nighttime. For some, especially those with circadian rhythm issues, it helps. But it’s not a magic bullet. Most melatonin supplements contain doses far higher than what the body naturally produces-sometimes 10 times more. That can throw off your natural rhythm even more. And unlike prescription drugs, they’re not tightly regulated. What’s on the label isn’t always what’s in the bottle.
The Only Treatment That Actually Works Long-Term
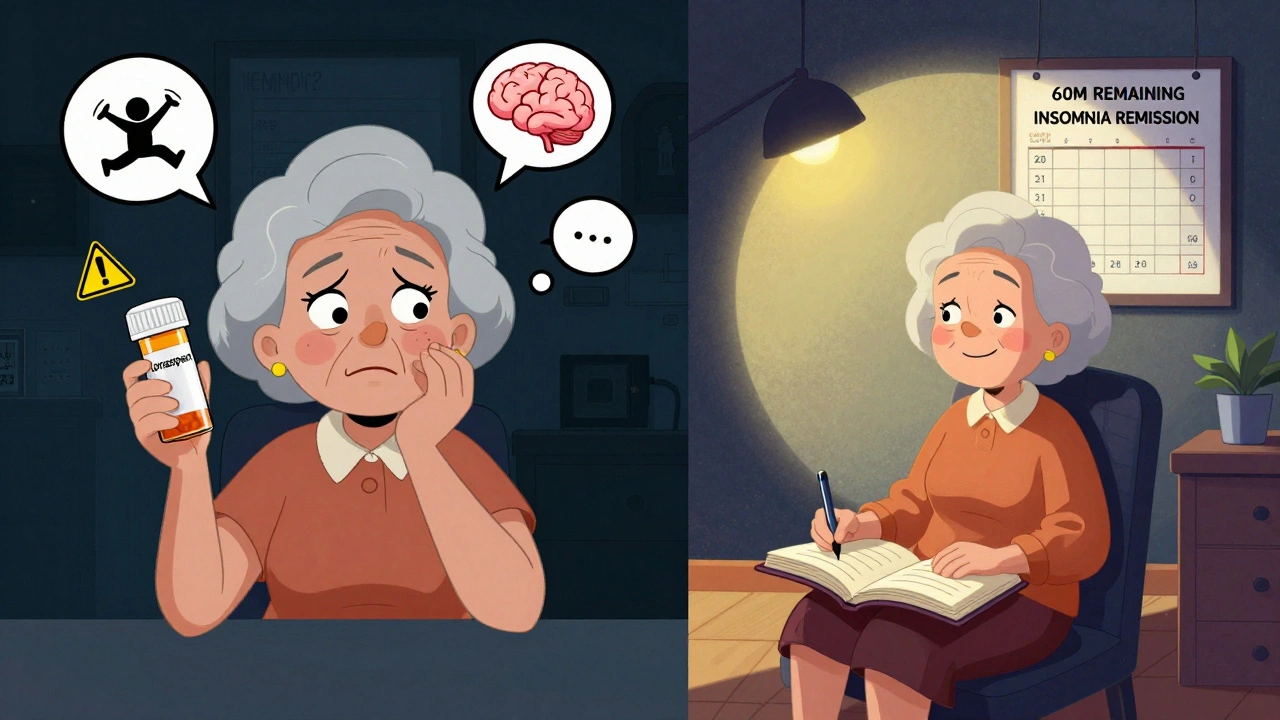
There’s one treatment that works better than any pill. It doesn’t cost hundreds of dollars. It doesn’t require a prescription. And it doesn’t carry the risk of dependence or cognitive decline. It’s called Cognitive Behavioral Therapy for Insomnia, or CBT-I.CBT-I isn’t about counting sheep or drinking chamomile tea. It’s a structured, evidence-based program that changes how you think about sleep. It teaches you to break the cycle of lying awake, stressing about not sleeping, and then doing things that make it worse-like checking the clock, napping during the day, or spending hours in bed awake.
Studies show CBT-I helps 70-80% of people with chronic insomnia. That’s better than any medication. And the benefits last. Unlike pills, which stop working after a few weeks, CBT-I teaches skills that stick. People who complete CBT-I report better sleep even five years later. WebMD data shows 78% of users who tried CBT-I had better long-term results than those who relied on medication alone.
The catch? It takes effort. It’s not instant. Most programs run 6-8 weeks. You have to keep a sleep diary. You have to limit time in bed. You have to face the discomfort of lying awake without reaching for a pill. That’s why many people give up. But those who stick with it? They rarely go back to meds.
New Options That Actually Make Sense
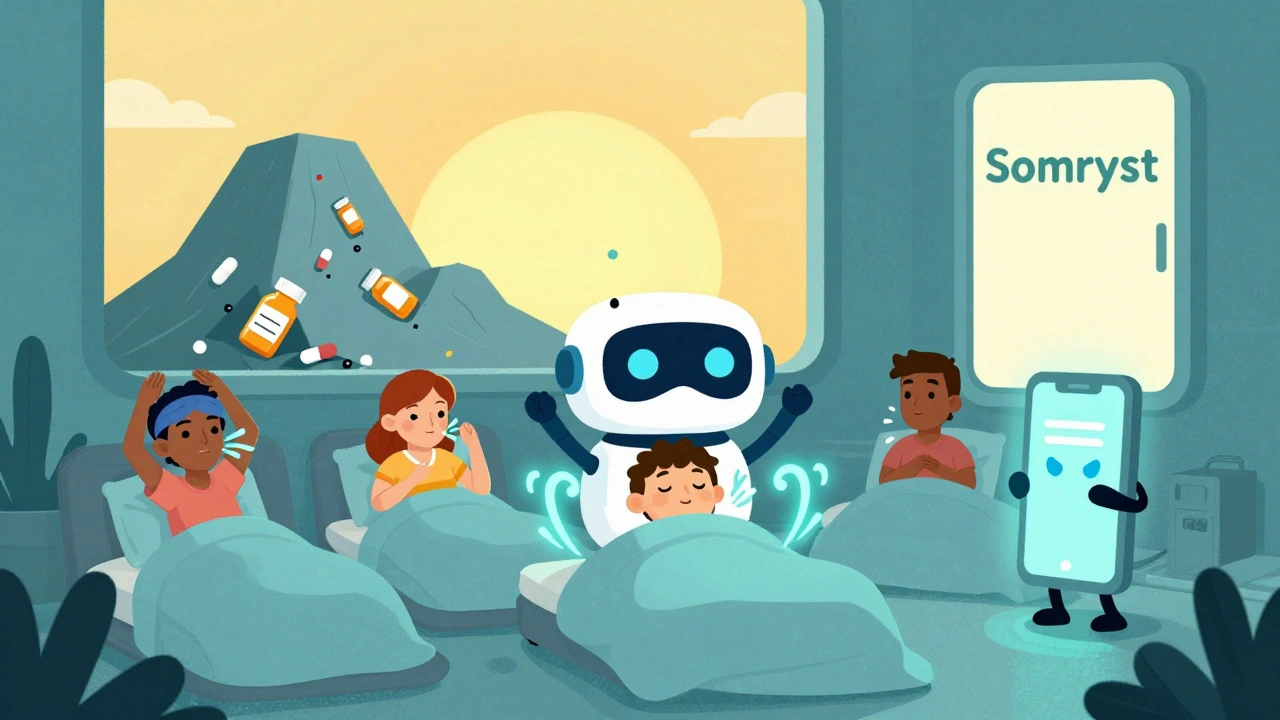
The future of sleep treatment isn’t more pills. It’s smarter ones-and non-drug tools.In 2020, the FDA approved Somryst, the first digital therapeutic for insomnia. It’s a prescription app that delivers full CBT-I through interactive modules. Clinical trials showed 60% of users achieved remission from insomnia. No pills. No side effects. Just guided behavioral change.
Then there’s daridorexant (Quviviq), approved in 2022. It’s not a sedative. It’s an orexin receptor antagonist. It works by blocking the brain’s wakefulness signal, not by shutting down the whole system. Early data shows less next-day drowsiness than zolpidem. It’s not a cure, but it’s a step in the right direction.
And while prescription sleep meds are still big business-$5.4 billion in 2022-growth is slowing. Meanwhile, digital CBT-I tools are growing at nearly 17% per year. Health systems are catching on. 73% now require prior authorization for sleep meds beyond 30 days. 68% require proof you’ve tried CBT-I first.
What to Do If You’re on Sleep Meds Right Now
If you’re taking a sleep medication, here’s what to do next:- Don’t stop cold. Abrupt withdrawal can cause severe rebound insomnia, anxiety, or seizures. Talk to your doctor about tapering.
- Ask about CBT-I. Your doctor may not bring it up, but you can. Say: “I want to try non-drug options first. Can you refer me to a CBT-I provider?”
- Track your sleep. Use a simple journal or app. Note when you go to bed, how long it takes to fall asleep, how many times you wake up, and how you feel in the morning.
- Eliminate alcohol. Mixing sleep meds with alcohol increases overdose risk by 300%. It also ruins sleep quality.
- Check your dose. Especially if you’re over 65. Many prescriptions are still written at outdated, too-high doses.
If you’re on a Z-drug like Ambien, ask if your dose is 5mg or lower. If you’re on a benzodiazepine, ask if it’s truly necessary. Many people take them for anxiety, not sleep-and there are better options for that too.
When Medication Might Still Be Necessary
Let’s be clear: sleep meds aren’t always the enemy. For someone with acute insomnia after a trauma, surgery, or major life event, a short course can be lifesaving. For people with severe depression and insomnia, a low-dose sedating antidepressant like doxepin might be the bridge they need to get to CBT-I.Dr. David Neubauer of Johns Hopkins says: “For certain populations, appropriate medication use remains essential-when combined with therapy.” That’s the key: combination. Medication as a temporary tool, not a long-term solution.
The goal isn’t to scare you off all sleep aids. It’s to make sure you’re not stuck on them because no one told you there was another way.
Final Thought: Sleep Is Not a Problem to Be Fixed
Sleep isn’t something you take a pill to fix. It’s a process. A rhythm. A natural function that responds to light, stress, routine, and mindset. Pills can help you fall asleep. But only you can teach your brain how to sleep well on its own.The best sleep you’ll ever have isn’t the one you get with a pill. It’s the one you earn by changing how you live, think, and rest.
Can sleep medications cause memory loss?
Yes. Both prescription sleep aids and OTC antihistamines like diphenhydramine can cause next-day memory problems, confusion, and even temporary amnesia. Some users report doing things while asleep-like driving or eating-with no memory of it afterward. This is especially common with Z-drugs like zolpidem. Long-term use of anticholinergic OTC meds is also linked to a 54% higher risk of dementia, according to JAMA Internal Medicine.
How long can you safely take sleep medications?
Clinical guidelines recommend using prescription sleep meds for no longer than 2 to 5 weeks. After that, effectiveness drops, and risks like dependence, tolerance, and next-day impairment rise. Even if you feel fine, your body is adapting. Long-term use is not supported by evidence and is strongly discouraged by the American Academy of Sleep Medicine.
Is melatonin safer than prescription sleep aids?
Melatonin is generally safer in the short term because it’s not addictive and doesn’t cause next-day drowsiness like benzodiazepines or Z-drugs. But it’s not a cure for insomnia. It helps regulate sleep timing, not deepen sleep. Many supplements contain doses far higher than needed, and quality isn’t regulated. It’s best for jet lag or shift work, not chronic insomnia.
Can you become addicted to sleeping pills?
Yes. While not everyone becomes addicted, physical dependence is common. You may find you need higher doses for the same effect, or you feel anxious if you miss a dose. Stopping suddenly can cause rebound insomnia, anxiety, or even seizures. Z-drugs like Ambien are classified as Schedule IV controlled substances because of their abuse potential. Dependence can develop in as little as four weeks with regular use.
What’s the best alternative to sleeping pills?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the most effective long-term alternative. It’s recommended as first-line treatment by the American Academy of Sleep Medicine. Digital CBT-I apps like Somryst are FDA-approved and show 60% remission rates. Other helpful strategies include maintaining a consistent sleep schedule, avoiding screens before bed, limiting caffeine after noon, and using your bed only for sleep and sex.
Why do doctors still prescribe sleep meds if they’re risky?
Many doctors prescribe them because they’re fast, familiar, and patients ask for them. CBT-I requires time, training, and referral networks that aren’t always available. Insurance often doesn’t cover CBT-I well, while pills are cheap and easy to write. But awareness is changing. More hospitals now require proof you’ve tried CBT-I before approving long-term prescriptions.
Are natural sleep aids like valerian root or magnesium effective?
Evidence is mixed. Some small studies suggest valerian root or magnesium might help mild sleep issues, but results aren’t consistent or strong enough to recommend them over CBT-I. Unlike prescription drugs, these supplements aren’t regulated for purity or dosage. They’re not risk-free-some interact with medications or cause digestive upset. Don’t assume “natural” means safe or effective.
What should I do if I want to stop taking sleep medication?
Talk to your doctor first. Stopping abruptly can be dangerous. A safe plan usually involves slowly reducing the dose by 25% every two weeks. During this time, start CBT-I or other behavioral strategies. Keep a sleep journal to track progress. Support groups and sleep coaches can help with motivation. Don’t try to quit alone-rebound insomnia is real, and having a plan makes all the difference.


Shayne Smith
December 6, 2025I used to take Ambien every night for years. One morning I woke up in the kitchen eating peanut butter straight from the jar with no memory of getting up. Scared the hell out of me. Stopped cold turkey and slept worse for a month, but now I don’t need it. CBT-I was a game changer. Just gotta stick with it.
Katie O'Connell
December 7, 2025The conflation of pharmacological intervention with moral failure is both reductive and ideologically driven. The assertion that CBT-I is universally superior ignores the neurobiological heterogeneity of insomnia. To dismiss medication as inherently dangerous is to privilege anecdotal narrative over clinical nuance.
Inna Borovik
December 8, 2025Let’s be real - 70% of people who try CBT-I drop out before week 3. The article makes it sound like everyone just needs to ‘try harder.’ Meanwhile, the real problem is the healthcare system doesn’t fund it properly. Doctors don’t have time. Insurance won’t cover it. So people take the pill because it’s the only option available to them.
Annie Gardiner
December 8, 2025You say sleep isn’t a problem to be fixed… but what if it is? What if your brain just needs a little help to shut off? Maybe the pill isn’t the villain - maybe it’s the system that made you feel like you need it in the first place. I’m not saying take it forever. I’m saying stop shaming people for using it.
Rashmi Gupta
December 8, 2025In India, people use melatonin like candy. No one checks doses. No one cares. My aunt took 10mg every night for 5 years. Now she forgets her own grandchildren’s names. This isn’t a Western problem. It’s a global one.
Andrew Frazier
December 10, 2025CBT-I? sounds like hippie nonsense. I work 60 hours a week, have two kids, and my wife snores like a chainsaw. You want me to sit there and journal my feelings instead of taking a pill that works? nah. i'll take the pill and keep my sanity. america doesn't need more therapy. it needs more sleep.
Kumar Shubhranshu
December 11, 2025Doctors prescribe because patients ask. Patients ask because ads tell them to. Ads tell them to because pharma pays. It’s a loop. CBT-I works but no one promotes it. Simple.
Mayur Panchamia
December 13, 2025You’re telling me to quit my Ambien... but you didn’t mention that the FDA-approved digital app costs $600?! And my insurance says ‘not medically necessary’? So now I’m supposed to pay out of pocket to fix a problem that was created by corporate greed and lazy medicine?! This isn’t advice - it’s a joke.
Karen Mitchell
December 13, 2025The suggestion that melatonin is ‘safe’ is dangerously misleading. The supplement industry is a regulatory wasteland. You cannot trust labels. You cannot trust purity. And yet, millions consume these substances daily with zero oversight. This is not wellness. It is negligence.
Geraldine Trainer-Cooper
December 14, 2025I stopped sleeping pills after my therapist said, 'You're not broken, you're just exhausted.' Took me 18 months. Had nights where I cried because I was so tired. But now? I sleep like a rock. Not because of a pill. Because I finally stopped fighting my body.
Nava Jothy
December 14, 2025I tried CBT-I. It was great... until my insurance dropped coverage after 4 sessions. Now I’m back on Lunesta. 😔 But at least I have a good playlist for bedtime. 🎧💤
Kenny Pakade
December 15, 2025The whole article reads like a corporate pamphlet from a wellness startup. CBT-I isn’t magic. It’s just a fancy way of saying ‘go to bed earlier.’ Meanwhile, real people are dying from sleep deprivation because they can’t afford to take time off. Stop preaching. Start fixing the system.