
Handling chemotherapy isn’t just about giving a patient a drug. It’s about protecting the person receiving it, the nurse giving it, the caregiver at home, and even the environment. One mistake-wrong dose, wrong patient, spilled liquid, or contaminated glove-can lead to serious harm. In 2024, the standards changed. The rules aren’t just suggestions anymore. They’re mandatory. And if you’re involved in cancer care, you need to know exactly what they are.
Why Chemotherapy Is Different From Other Medications
Most drugs are safe to touch. Chemotherapy isn’t. Antineoplastic agents are designed to kill fast-growing cells. That’s why they work against cancer. But they don’t know the difference between a cancer cell and a healthy one-like the ones in your skin, hair, or bone marrow. Even tiny amounts of these drugs can cause long-term damage. Nurses who handle them without proper protection have higher rates of miscarriage, infertility, and even leukemia. Patients can get sick from accidental exposure. And if a spill isn’t cleaned correctly, the contamination lingers for days.
These aren’t hypothetical risks. A 2022 NCCN safety report found that 18% of chemotherapy-related adverse events were due to patient misidentification. Another study showed that 78% of oncology nurses had visible drug contamination on their gloves after handling just one dose. This isn’t rare. It’s routine-unless you stop it.
The 2024 ASCO/ONS Safety Standards: What Changed
The American Society of Clinical Oncology and the Oncology Nursing Society updated their guidelines in early 2024. This wasn’t a minor tweak. It was a full overhaul. The term "chemotherapy" was replaced with "antineoplastic therapy" because now, most treatments aren’t traditional chemo. They’re targeted drugs, immunotherapies, antibody-drug conjugates-all of which carry similar risks.
The new standards break down into four key areas:
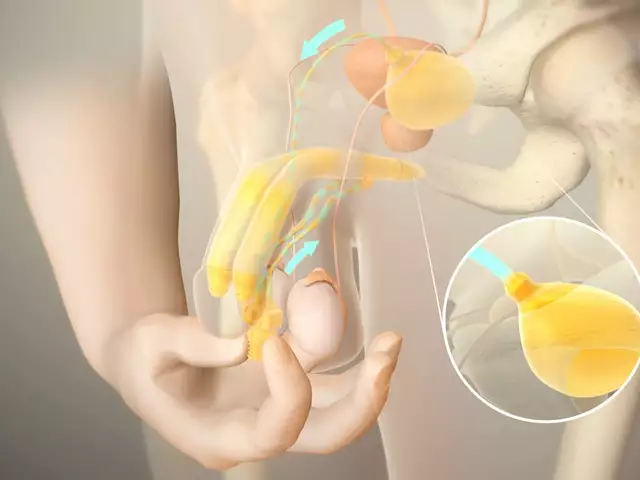
- Safe Environment: Facilities must have designated areas with negative air pressure, closed-system transfer devices (CSTDs), and spill kits readily available. CSTDs prevent vapors and droplets from escaping during drug transfer. They’re not optional anymore.
- Patient Consent and Education: Before treatment, patients must be told the exact name of the drug, the dose, how long treatment will last, and what side effects to expect. This isn’t just paperwork. It’s part of safety. If a patient doesn’t understand what they’re getting, they can’t spot a mistake.
- Ordering, Preparing, and Administering: This is where the biggest change happened. A fourth verification step is now required-done right at the patient’s bedside. Two licensed staff members must check the patient’s name, date of birth, drug name, dose, route, and time. All four checks must be completed before the IV starts. And they must be done in front of the patient.
- Monitoring During and After: New protocols now require hospitals to have antidotes for cytokine release syndrome (CRS) ready at all times. CRS can happen with immunotherapies like CAR-T or bispecific antibodies. It causes high fever, low blood pressure, and breathing trouble. If not treated within 30 minutes, mortality jumps to 12-15%.
Personal Protective Equipment (PPE): What You Need and Why
Wearing gloves and a gown isn’t enough. You need the right kind.
- Double Gloves: Must be chemotherapy-tested. Regular exam gloves? They break down in minutes when exposed to drugs like carmustine or thiotepa. NIOSH-certified double gloves reduce skin exposure by 95%.
- Impermeable Gowns: Not just any lab coat. Must be tested to resist permeation by antineoplastic agents. Cloth gowns? They’re useless.
- Eyes and Respiratory Protection: If you’re mixing drugs or cleaning a spill, you need goggles or a face shield. If aerosols are possible (like with oral chemo powders), you need an N95 mask or better.
- Disposal: Every piece of PPE used during handling is contaminated. It doesn’t go in the regular trash. It goes in a red hazardous waste bin labeled for antineoplastic agents.
One study found that nurses who changed gloves every 30 minutes had 80% less hand contamination than those who reused them. That’s not a suggestion. That’s a proven safety rule.

Home Chemotherapy: The Hidden Risk
More patients are getting chemo at home now. It’s convenient. But it’s dangerous if no one’s watching.
The American Cancer Society found that 22% of home care incidents involve improper disposal of chemo waste-like used syringes, empty bottles, or even soiled tissues. Seventeen percent involve spills that weren’t cleaned with the right kit. And 65% of caregivers say they feel unprepared, even after receiving training materials.
Here’s what home caregivers must do:
- Store all drugs in a locked, child-proof container, away from pets and other people.
- Use a chemotherapy spill kit immediately if anything leaks. Never use paper towels or regular cleaners.
- Wear gloves when handling bodily fluids for 48-72 hours after treatment. That includes urine, vomit, sweat, or blood.
- Dispose of sharps in a FDA-cleared sharps container-not a soda bottle.
- Wash hands immediately after handling anything related to treatment.
Facilities that use the ASCO-developed "Chemotherapy Safety at Home" toolkit saw a 41% drop in caregiver safety concerns. That’s not magic. That’s clear instructions.
Costs and Barriers to Full Compliance
Implementing these standards isn’t cheap. A medium-sized clinic needs $22,000-$35,000 for facility upgrades. Another $8,500-$12,000 for staff training. Then $4,200-$6,800 a year just for gloves, gowns, and waste disposal.
And it’s not just money. Many rural clinics can’t afford closed-system transfer devices. Dr. Sarah Temkin from UVA Health found that 43% of rural programs can’t meet CSTD requirements. That means patients in those areas get the same drugs-but with less protection for the staff giving them.
Electronic health records (EHRs) are another bottleneck. Sixty-seven percent of clinics need custom software to support the four-step verification process. That costs $15,000-$40,000 per system. Many still rely on paper checklists-slow, error-prone, and hard to audit.
OSHA issued 142 citations in 2022 for unsafe chemo handling. The average fine? $14,250. Facilities that skip steps aren’t just risking lives-they’re risking their licenses.
What’s Working: Real Stories From the Front Lines
Not all stories are grim. In a 347-facility survey, 78% of oncology nurses said their confidence went up after full implementation of the 2024 standards. Why? The bedside verification step. "Before, I’d double-check the name on the chart," said one nurse in Ohio. "Now I look the patient in the eye and ask them to say their name. That changes everything."
One facility in Texas cut near-miss errors by 52% after introducing the four-step check. Another reduced occupational exposures by 78% in two years.
But not everyone agrees. On Reddit, a nurse named "ChemoRN2020" wrote: "The fourth check adds 7-10 minutes per patient. We’re already understaffed. Errors haven’t gone down here. We’re just tired."
That’s the tension. Safety takes time. And time is scarce. But the data says: when done right, it saves lives.
What’s Coming Next
The National Comprehensive Cancer Network (NCCN) will start requiring proof of fourth verification and CRS protocols for facility accreditation starting January 2025. That means if you’re not compliant, you won’t be accredited.
By 2026, a national certification for chemotherapy administration staff is expected. Think of it like a license to handle these drugs.
Pilot programs are testing AI tools that scan patient IDs, drug labels, and doses in real time-cutting down manual checks. Early results show a 30% reduction in verification time.
And new drugs are coming. Bispecific antibodies, antibody-drug conjugates-each has unique handling needs. The 2024 standards already have gaps here. The next update will need to catch up.
Bottom Line: Safety Isn’t Optional
Chemotherapy is powerful. It can save lives. But it can also destroy them-if handled carelessly. The 2024 standards exist because people got hurt. Nurses got sick. Patients got the wrong dose. Caregivers didn’t know what to do.
There’s no room for shortcuts. Double gloves. Two identifiers. Bedside verification. Spill kits. Proper disposal. These aren’t bureaucratic hoops. They’re the bare minimum to keep everyone safe.
If you’re a nurse, a pharmacist, a doctor, or a caregiver-you’re part of this chain. One link breaks, and someone pays the price. Don’t assume someone else will handle it. Don’t wait for an audit. Don’t hope for the best.
Do it right. Every time.
Do I need to wear double gloves for all chemotherapy drugs?
Yes-for drugs classified as hazardous by NIOSH, including most antineoplastic agents. Double chemotherapy-tested gloves are required for handling drugs like carmustine, thiotepa, and cyclophosphamide. Even if you think the risk is low, contamination studies show that single gloves often break down within minutes. Always use double gloves unless the drug’s safety data sheet says otherwise.
What happens if I spill chemotherapy on the floor?
Never use paper towels or regular cleaners. Use a certified chemotherapy spill kit, which includes impermeable gloves, absorbent pads, and a disposal bag. Put on double gloves and a gown first. Contain the spill, then carefully absorb it. Place all materials in a hazardous waste container labeled for antineoplastic agents. Clean the area again with a detergent solution. Document the spill and report it to your safety officer. The drug can remain active on surfaces for days.
Can a patient take chemotherapy at home safely?
Yes-but only with proper training and tools. The patient and caregiver must receive hands-on instruction from a trained oncology nurse. They need a locked storage container, a spill kit, PPE for handling bodily fluids, and a sharps container. They must know how to dispose of waste and what symptoms require immediate medical help. Facilities using the ASCO "Chemotherapy Safety at Home" toolkit report 41% fewer safety concerns from caregivers.
Why is the fourth verification step so important?
Patient misidentification caused 18% of chemotherapy-related adverse events in 2022. The fourth verification-done in front of the patient with two licensed staff using two identifiers (name and date of birth)-cuts that risk dramatically. It’s the last chance to catch a mistake before the drug enters the body. It’s not just a formality. It’s a life-saving step.
Are all chemotherapy drugs equally dangerous to handle?
No. NIOSH classifies hazardous drugs into five groups based on toxicity, exposure risk, and potency. Drugs like doxorubicin and cisplatin are high-risk. Others, like some oral targeted therapies, are lower risk-but still require gloves and proper disposal. Never assume a drug is safe because it’s a pill. Always check the drug’s safety profile and follow the facility’s hazard classification list.
What should I do if I think I’ve been exposed to chemotherapy?
Wash the exposed area immediately with soap and water. Remove contaminated clothing. Report the exposure to your supervisor and occupational health department-even if you feel fine. Some effects are delayed. Your facility should have a formal exposure incident protocol. Most don’t require you to prove fault-just report it. Only 41% of exposed workers report incidents because they fear backlash. Don’t be silent. Your health matters.
How often do staff need training on chemotherapy safety?
Initial training requires 8-12 hours, including a written exam (minimum 85% pass) and a hands-on skills demonstration. After that, annual 4-hour refreshers are mandatory. Training must be updated whenever new drugs, protocols, or equipment are introduced. Simply watching a video isn’t enough. You must demonstrate competency in real scenarios.
If you're managing a clinic, start with a gap analysis: Do you have CSTDs? Are staff trained? Is your EHR set up for four-step verification? If you're a caregiver, ask your oncology team for the "Chemotherapy Safety at Home" guide. If you're a nurse, never skip the verification. This isn’t about rules. It’s about respect-for the patient, for your colleagues, and for yourself.



Allen Davidson
January 16, 2026Just saw a nurse at my mom's clinic skip the double gloves because she was 'in a hurry.' She didn't get sick, but I'll never forget the look on her face when the safety officer pulled her aside. This isn't about rules-it's about not being the reason someone loses their hair for the second time, this time from your mistake.
Nick Cole
January 16, 2026My wife's oncology nurse started doing the bedside verification with her name and DOB out loud. My wife, who’s usually quiet as a mouse, started correcting her when she got the DOB wrong. That’s the moment it clicked-this isn’t just for the staff. It’s for us too.
Christina Bilotti
January 18, 2026Oh wow, another 12-page manifesto on how to not poison people. Did you also include a flowchart for how to properly cry when you realize your hospital can't afford CSTDs? I'm sure the nurses in rural Alabama are just dying to read this while they're using expired gloves.
brooke wright
January 18, 2026I work in home care and my client’s husband used a soda bottle for sharps disposal because he didn’t know better. I found it in the garage next to the lawnmower. I cried. I didn’t tell anyone. But now I bring extra containers every visit. No one should have to clean up someone else’s ignorance.
Henry Ip
January 20, 2026Bedside verification works because it turns a checklist into a human moment. I used to hate the extra time. Now I wait for the patient to say their name back. Sometimes they laugh. Sometimes they’re scared. Either way, they’re part of the team now. That’s worth every second.
Cheryl Griffith
January 21, 2026My sister’s chemo nurse changed gloves every 30 minutes like the article said. She didn’t say anything. Just did it. I asked why. She said, 'Because I don’t want to be the reason your sister gets sick again.' I’ll never forget that. Not because of the rule. Because of the heart behind it.
Kasey Summerer
January 22, 2026USA thinks it's the only country with chemo safety standards. Meanwhile, Germany uses automated verification bots and Canada has national PPE subsidies. We're still arguing over whether to use N95s or surgical masks. 🤦♂️
kanchan tiwari
January 24, 2026THIS IS A BIG PHARMA COVERUP. They don't want you to know that chemotherapy was designed to make nurses sick so they'd stay quiet while patients died. The '2024 standards' are just a distraction. The real danger? The microchips in the IV bags. I've seen the footage. They're watching us through the gloves. Someone's gotta speak up.
Bobbi-Marie Nova
January 25, 2026Okay but let’s be real-no one’s gonna do all this if the hospital is running on fumes and the EHR crashes every 3 minutes. We get it, safety’s important. But maybe fix the damn system first? Just saying. 🙃
john Mccoskey
January 27, 2026The entire framework of chemotherapy safety is built on a fallacy: that human beings can be trusted with lethal substances. The four-step verification? A bandage on a hemorrhage. The real solution is automation. AI-driven barcode scanning. Robotic dispensing. Human error isn't a variable-it's a constant. And we're pretending we can outthink biology, chemistry, and fatigue with checklists. This isn't progress. It's tragic optimism.
Ryan Hutchison
January 29, 2026Why are we letting foreigners dictate how we handle medicine? The ASCO standards? More like ASIA standards. We’ve got American nurses who’ve been doing this for 20 years. They don’t need some newfangled CSTD to do their job. We need to trust our people, not buy expensive toys from Silicon Valley.
Samyak Shertok
January 30, 2026Everyone’s obsessed with the fourth verification step like it’s the Ten Commandments. But what about the fifth? The one where you ask the patient if they’re okay with this drug because maybe they don’t want to die from it? Or the sixth? Where you ask if they’ve ever been lied to by a doctor before? The real safety protocol isn’t in the checklist-it’s in the silence between the questions.