Smoking and Your Health: Essential Facts and Tips to Quit
If you light up regularly, you’ve probably heard that smoking is bad. But what does “bad” really mean for your body and the medicines you take? In this guide we’ll break down the biggest ways smoking messes with your health, how it can change drug effectiveness, and practical steps to cut back or quit without feeling lost.
How Smoking Changes How Your Medications Work
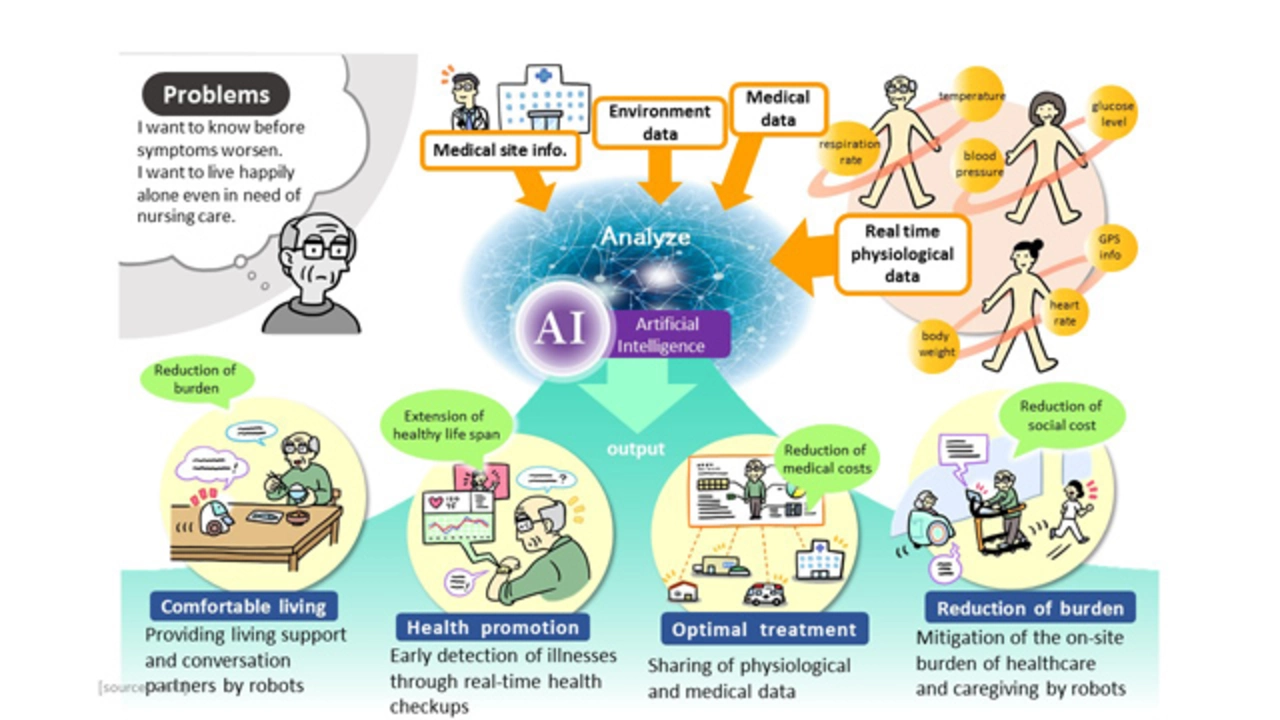
When you smoke, chemicals like nicotine and tar rush into your bloodstream. Those compounds speed up the liver’s enzyme system, especially CYP1A2. That means drugs such as certain antidepressants, blood thinners, and even some antibiotics can be cleared faster, leaving them less effective. For example, a smoker may need a higher dose of a medication like clozapine to reach therapeutic levels, while a non‑smoker would feel the same effect with less.
On the flip side, smoking can also increase side effects for drugs that are broken down more slowly. Think about asthma inhalers – nicotine can irritate airways, making you think your inhaler isn’t working when it actually is. Knowing these interactions helps you talk to a doctor and avoid unexpected flare‑ups.
Quick Wins to Reduce Smoking Harm
You don’t have to quit cold turkey if that feels overwhelming. Start by cutting the number of cigarettes you smoke each day. Even shaving off one or two can lower heart rate and improve lung function within weeks. Pair this reduction with a simple habit swap: replace a cigarette break with a short walk, a glass of water, or chewing sugar‑free gum.
Another easy trick is to change your smoking environment. If you usually smoke after meals, try brushing your teeth right away – the fresh taste makes a cigarette feel less appealing. Keep nicotine replacement products (like patches or lozenges) handy for moments when cravings hit hard; they deliver a steadier dose of nicotine without the harmful smoke.
Long‑Term Strategies to Quit for Good
When you’re ready for a bigger change, set a quit date and tell friends or family. Social support adds accountability and makes it easier to stay on track. Use reputable apps that track cravings, give daily tips, and celebrate milestones – seeing progress in numbers can be surprisingly motivating.
If cravings feel intense, consider talking to a healthcare professional about prescription aids such as varenicline or bupropion. These medications target the brain’s nicotine receptors, reducing the urge to smoke while easing withdrawal symptoms. Combine them with counseling (online or in‑person) for the best success rate.
Finally, remember that quitting is a marathon, not a sprint. Slip‑ups happen; they don’t erase all your progress. Each cigarette you avoid lowers your risk of heart disease, lung cancer, and improves how your body processes medication. Keep focusing on the small wins, and over time the big health benefits will become clear.