Doxercalciferol: What It Is, How It Works, and What You Need to Know
When your body can't make enough active vitamin D or your parathyroid glands aren't working right, doxercalciferol, a synthetic form of vitamin D2 used to regulate calcium and parathyroid hormone levels. Also known as 1α-hydroxyvitamin D2, it helps your intestines absorb calcium and tells your bones to release it when needed. Unlike regular vitamin D supplements, doxercalciferol is already partially activated—your body doesn’t need to convert it in the kidneys. That’s why it’s often prescribed for people with kidney disease, where that conversion process is broken.
This drug is mostly used in two situations: hypoparathyroidism, a condition where the parathyroid glands don’t make enough hormone to control calcium, and renal osteodystrophy, bone damage caused by long-term kidney failure. In both cases, calcium levels drop too low, and parathyroid hormone rises too high, leading to weak bones, muscle cramps, and even heart problems. Doxercalciferol steps in to fix that balance without overworking the kidneys. It’s not a cure, but it’s a tool that helps people live better with these chronic conditions.
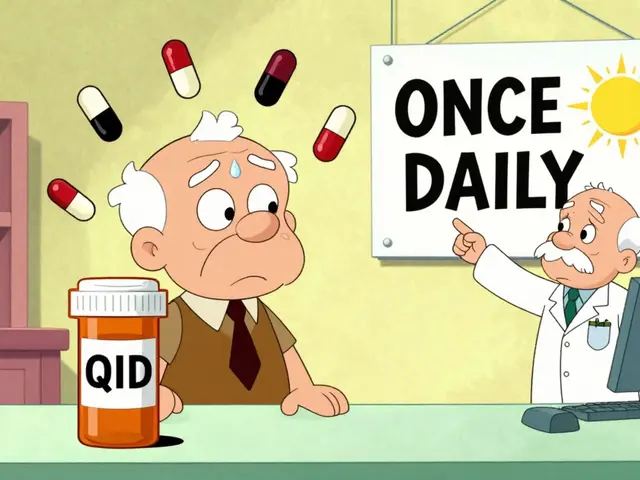
It’s not the only option. Some patients use calcitriol, another activated vitamin D, but doxercalciferol has a lower risk of raising blood calcium too high—a common side effect that can be dangerous. It’s also used when other forms of vitamin D don’t work well due to kidney damage. But it’s not for everyone. If you have high calcium levels already, or if you’re allergic to vitamin D compounds, this drug can make things worse. Your doctor will check your blood regularly to make sure the dose is just right.
What you’ll find in the posts below aren’t direct reviews of doxercalciferol—there aren’t any—but you’ll see how it fits into the bigger picture of drug interactions, kidney-related treatments, and calcium management. You’ll read about how other drugs like statins or PPIs affect mineral balance, how antibiotics can trigger dangerous reactions in vulnerable patients, and how even common painkillers need careful handling in older adults. These aren’t random topics. They’re all connected by one thing: how medications interact with your body’s chemistry, especially when your organs aren’t working perfectly. Whether you’re managing a chronic condition, caring for someone who is, or just trying to understand why your doctor picked one drug over another, this collection gives you real, practical context—not just theory.