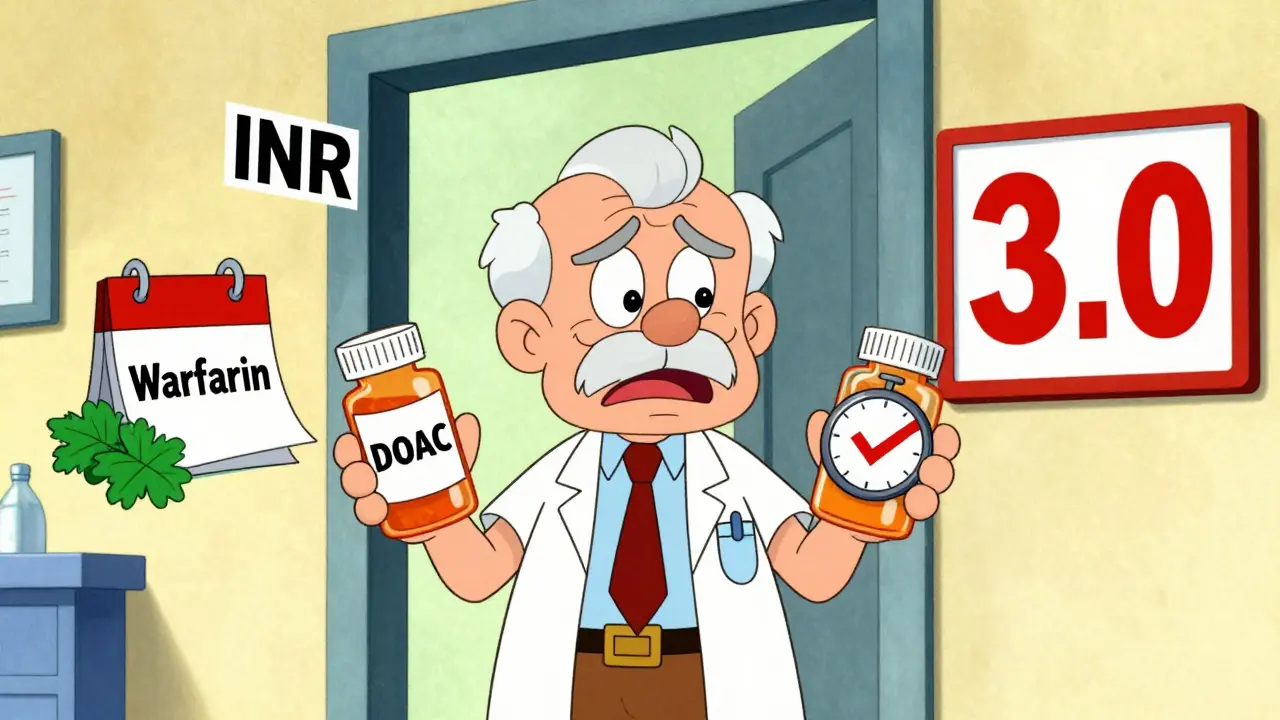
Warfarin to DOAC Switch Calculator
INR-Based Switching Guide
This tool helps determine when it's safe to switch from warfarin to a DOAC based on your INR level. Always consult with your healthcare provider before making any changes to your anticoagulant therapy.
Switching from warfarin to a DOAC isn’t just swapping one pill for another. It’s a careful, timed process that can mean the difference between staying safe and facing serious risks like stroke or dangerous bleeding. If you’ve been on warfarin for years - with weekly blood tests, dietary restrictions, and constant worry about interactions - the idea of switching to a DOAC sounds like a dream. Fewer blood tests. No more avoiding kale. But this switch has traps. Get it wrong, and you could end up in the hospital.
Why Do People Switch from Warfarin to DOACs?
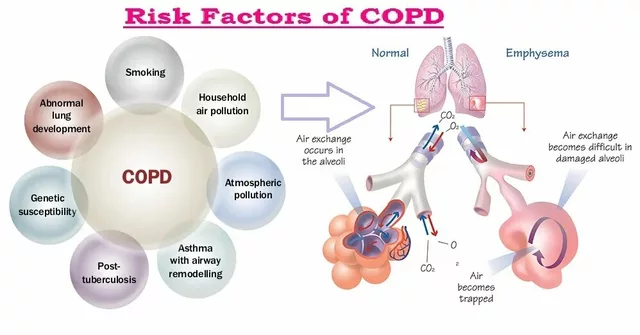
Warfarin has been the go-to blood thinner since the 1950s. It works, but it’s messy. You need regular INR tests - often every 1 to 4 weeks - to make sure your blood isn’t too thin or too thick. Your diet matters too. Vitamin K in leafy greens can throw off your dose. And dozens of medications, from antibiotics to herbal supplements, can interfere with how warfarin works. DOACs - dabigatran, rivaroxaban, apixaban, and edoxaban - changed the game. They don’t need routine blood tests. They have fewer food and drug interactions. And for most people, they’re just as good at preventing strokes, with lower risks of brain bleeds. In clinical trials, DOACs cut intracranial hemorrhage by about 30% compared to warfarin. That’s not small. For someone over 70, it could mean the difference between staying independent and needing long-term care after a bleed.When Is It Safe to Switch?
Not everyone can switch. There are hard rules. If you have a mechanical heart valve, don’t even consider it. DOACs don’t work for those cases. Same if you’re pregnant or breastfeeding. Severe liver disease (Child-Pugh Class C) is another no-go. Renal function matters too. If your creatinine clearance (CrCl) is below 15-30 mL/min, depending on the DOAC, you might not be a candidate. For example, dabigatran and edoxaban are cleared mostly by the kidneys. If your kidneys are weak, the drug builds up and raises bleeding risk. Apixaban is a bit more forgiving in mild-to-moderate kidney issues, but you still need to check. The biggest mistake? Switching without checking your INR. You can’t just stop warfarin and start a DOAC on the same day. The timing depends on your last INR result.- If your INR is ≤2.0: Start the DOAC right away.
- If your INR is 2.0-2.5: Start the DOAC the same day or next day.
- If your INR is 2.5-3.0: Wait 1-3 days, retest, then switch.
- If your INR is ≥3.0: Delay the switch. Wait 3-5 days and retest.
What Happens During the Switch?
The transition window is narrow. Too early, and you risk clotting. Too late, and you risk bleeding. For example, if your INR is 2.3, you might take your last warfarin dose at 8 a.m. on Monday, then take your first DOAC dose at 8 a.m. on Tuesday. No gap. No overlap. That’s ideal. But if your INR is 2.8 on Monday, you wait. Retest on Wednesday. If it’s down to 2.1, you start the DOAC then. Waiting longer than needed increases your stroke risk - especially if you have atrial fibrillation. A 2021 study from the Minnesota Cardiovascular Conference found that stopping anticoagulation, even briefly, spikes stroke risk in AFib patients. That’s why timing matters more than convenience. Some clinicians, especially in areas without easy access to INR testing, wait 2-3 days after the last warfarin dose before starting the DOAC. But this is a backup plan. It’s not ideal. If your INR is still high after 3 days - common in older adults or those with liver issues - you might need to wait longer. Don’t guess. Test.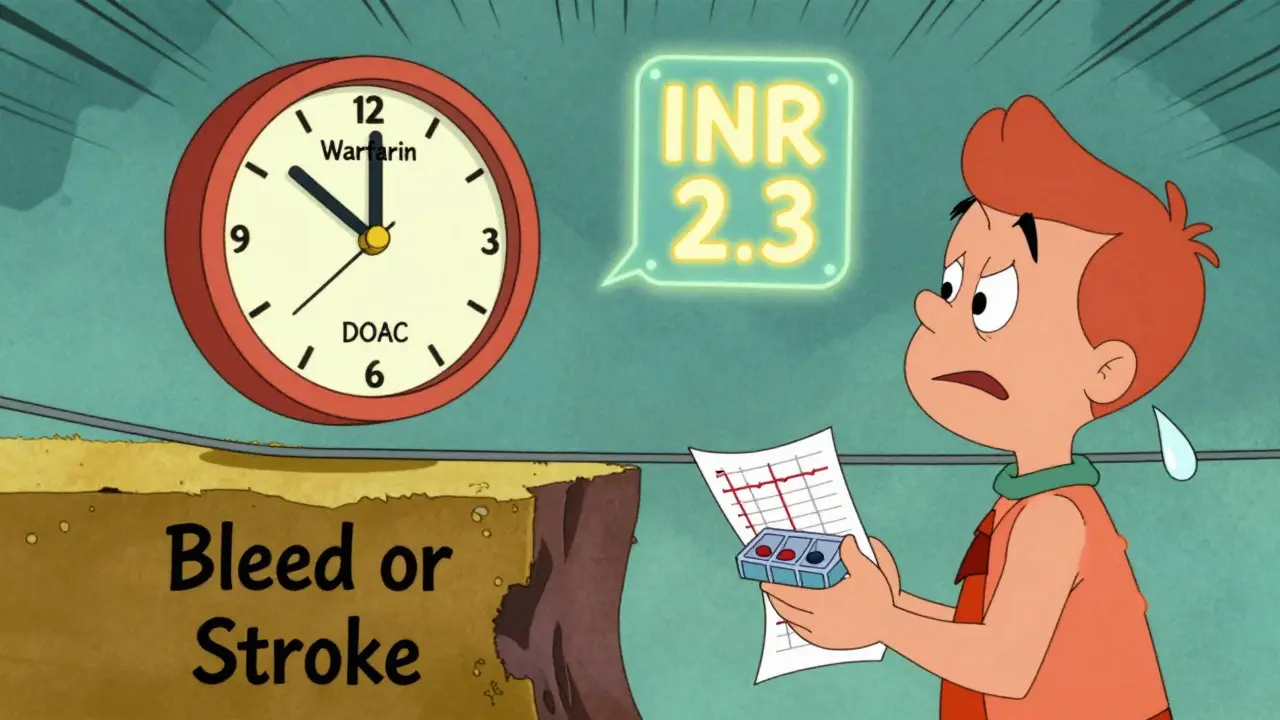
Side Effects You Might Not Expect
DOACs are generally safer than warfarin, but they’re not harmless. The most common issue during the switch? Gastrointestinal bleeding. It’s not rare. Some patients report stomach pain, dark stools, or vomiting blood in the first few weeks after switching. This often happens because the anticoagulant effects of warfarin haven’t fully worn off when the DOAC kicks in. Also, DOACs can raise your INR slightly - even though they don’t work through vitamin K. That’s why some labs report falsely high INR values after switching. Don’t panic. Your doctor should know this. Don’t adjust your DOAC dose based on an INR result unless you’re told to. Another hidden risk: forgetting to take your DOAC. Warfarin’s long half-life meant you could miss a dose and still be protected. DOACs? They’re gone in 12-24 hours. Miss one dose of apixaban or rivaroxaban, and your protection drops fast. That’s why adherence is non-negotiable. Set phone alarms. Use pill organizers. Talk to your pharmacist about dosette boxes - most DOACs can go in them, except dabigatran. That one’s moisture-sensitive. Keep it in the original blister pack.Special Populations: What You Need to Know
If you weigh less than 60 kg or more than 150 kg, you were mostly left out of the original DOAC trials. That doesn’t mean you can’t switch - but you need extra care. Your doctor should check your kidney function, body weight, and possibly adjust the dose. For example, apixaban is often reduced to 2.5 mg twice daily if you’re over 80, weigh under 60 kg, or have a creatinine level above 1.5 mg/dL. Kidney function changes over time. Even if your CrCl was fine when you switched, get it checked every 6-12 months. A decline from 60 to 40 mL/min might mean you need a lower dose. Don’t assume your dose stays the same forever. If you’re scheduled for surgery or a dental procedure, plan ahead. DOACs need to be stopped before procedures - but not too early. For a low-risk procedure like a tooth extraction, someone with normal kidney function (CrCl >90 mL/min) on dabigatran should stop 24 hours before. If your CrCl is only 45 mL/min and you’re having major surgery, you might need to stop 96-108 hours ahead. Your surgeon and pharmacist should coordinate this. Don’t leave it to chance.What About Reversing DOACs?
If you bleed badly, can you reverse the DOAC? Yes - but only for some. For dabigatran, there’s idarucizumab. It works fast. For rivaroxaban and apixaban, there’s andexanet alfa. It’s expensive and not always available. For edoxaban, no specific reversal agent exists. In emergencies, doctors use activated charcoal (if the pill was taken recently), prothrombin complex concentrate (PCC), or even fresh frozen plasma. But none of these work as well as the specific antidotes. That’s why it’s critical to carry an anticoagulant alert card. If you’re in an accident and unconscious, paramedics need to know you’re on a DOAC. And which one. Keep the card in your wallet. Tell your family. Your pharmacist can give you one.
How to Make the Switch Work for You
Successful switching isn’t just about the doctor’s prescription. It’s about you.- Get your bloodwork done: INR, creatinine, liver enzymes - all within the last 6 months. If not, get them done before switching.
- Calculate your CrCl using the Cockcroft-Gault formula. Your doctor should do this, but know your number.
- Ask for a patient information leaflet on your new DOAC. Know the side effects, what to avoid, and when to call for help.
- Use a pill organizer - unless you’re on dabigatran. Keep that one in its original packaging.
- Set daily reminders. Don’t rely on memory.
- Book a follow-up with your pharmacist 2-4 weeks after switching. Many pharmacies offer free New Medicine Service checks.
What If the Switch Doesn’t Go Right?
Sometimes, despite doing everything right, things go sideways. Maybe you had a bleed. Maybe your INR stayed high after switching. Maybe you developed a rash or stomach pain that won’t go away. Don’t stop the DOAC on your own. Call your doctor. You might need to switch back to warfarin - but that’s another complex transition. Reversing from DOAC to warfarin requires overlapping with a short-acting anticoagulant like heparin until warfarin becomes effective. That’s not something to try at home. If you’re unsure, ask for a referral to an anticoagulation clinic. These specialized services exist for a reason. They track INR, adjust doses, and handle complications. Even if you’re on a DOAC now, having access to that expertise gives you peace of mind.Final Thoughts: Is Switching Worth It?
For most people with non-valvular atrial fibrillation, deep vein thrombosis, or pulmonary embolism - yes. DOACs are easier, safer, and just as effective. But only if the switch is done right. It’s not about convenience. It’s about precision. A missed INR test. A wrong timing. A forgotten dose. These aren’t small errors. They can lead to strokes, bleeds, or death. If your doctor suggests switching, ask: "What’s my current INR? What’s my kidney function? What’s the exact timing for stopping warfarin and starting the DOAC? What do I do if I miss a dose?" If they can’t answer clearly, get a second opinion. This isn’t a decision to rush. It’s a decision to do right.Can I switch from warfarin to a DOAC if I have atrial fibrillation?
Yes, most people with non-valvular atrial fibrillation are good candidates for switching to a DOAC. DOACs are actually preferred over warfarin in this group because they reduce the risk of stroke and brain bleeds. But you must have your INR checked before switching, and your kidney function must be assessed. If you have a mechanical heart valve, DOACs are not an option.
What happens if I miss a dose of my DOAC?
If you miss a dose of your DOAC, take it as soon as you remember - but only if it’s still the same day. If it’s already the next day, skip the missed dose and take your next one at the regular time. Never double up. DOACs leave your system quickly - within 12 to 24 hours - so missing a dose leaves you unprotected. Consistency matters more than with warfarin.
Do I still need blood tests after switching to a DOAC?
You don’t need routine INR tests anymore, which is one of the biggest benefits. But you still need occasional blood work - especially kidney function tests (creatinine and eGFR) every 6 to 12 months. Your liver function and complete blood count may also be checked annually. These aren’t for dosing - they’re to make sure your body is handling the drug safely.
Can I take other medications while on a DOAC?
Yes, but you need to be careful. Some drugs - like certain antibiotics (e.g., clarithromycin), antifungals, and seizure medications - can interact with DOACs and increase bleeding risk. Always tell your doctor or pharmacist about everything you take, including over-the-counter painkillers, herbal supplements, and vitamins. NSAIDs like ibuprofen can increase stomach bleeding risk when combined with DOACs. Stick to paracetamol (acetaminophen) if you need pain relief.
Is it safe to switch if I’m over 75?
Age alone isn’t a barrier. Many people over 75 switch successfully. But older adults often have reduced kidney function, lower body weight, and are on multiple medications - all of which raise bleeding risk. Your doctor should check your CrCl, weight, and medication list carefully. For apixaban, a lower dose (2.5 mg twice daily) is often used in patients over 80 or weighing under 60 kg. Close monitoring in the first few weeks is recommended.
What if I need emergency surgery?
If you need emergency surgery, tell the medical team you’re on a DOAC and which one. They may use reversal agents like idarucizumab (for dabigatran) or andexanet alfa (for factor Xa inhibitors like rivaroxaban and apixaban). If those aren’t available, they may use prothrombin complex concentrate (PCC). Time matters - the sooner they know, the better they can act. Always carry your anticoagulant alert card.


Gregory Parschauer
January 15, 2026Let’s be real - if you’re switching from warfarin to a DOAC without a full renal workup and INR trajectory analysis, you’re not managing anticoagulation, you’re playing Russian roulette with intracranial hemorrhage risk. The literature is unequivocal: DOACs reduce cerebral bleeds by 30%, but only when the transition window is calibrated to your pharmacokinetic profile. Skipping the CrCl check? That’s not negligence - that’s malpractice dressed up as convenience. And don’t get me started on patients who think ‘fewer blood tests’ means ‘no monitoring.’ You still need annual LFTs, CBCs, and eGFR tracking. This isn’t a upgrade - it’s a paradigm shift requiring clinical rigor.
Robin Williams
January 15, 2026bro i switched last year and it was like night and day. no more weekly finger pricks, no more stressing over spinach, just pop the pill and go. i forgot my dose once and panicked for 2 hours, then realized - oh right, this isn’t warfarin. i took it the next day and lived. my cardiologist said i’m low risk so he didn’t even want me to check my kidneys every 6 months but i did anyway. best decision ever. peace of mind is worth a little extra blood draw.
Scottie Baker
January 17, 2026you people are overcomplicating this. i’m 78, on apixaban, weigh 58kg, and my kidneys are garbage - CrCl 38. i missed a dose once because my phone died. i didn’t die. i didn’t stroke. i just took the next one. doctors act like we’re all gonna bleed out if we blink wrong. i’ve been on this stuff for 3 years. no GI bleed, no clots, no hospital trips. if you’re scared, stay on warfarin. but don’t scare the rest of us with your jargon-fueled panic.
Anny Kaettano
January 17, 2026Hi everyone - I’m a clinical pharmacist and I want to say thank you to the person who wrote this. It’s so rare to see a post that doesn’t just list facts but actually walks people through the emotional and practical weight of this transition. For so many of us, especially older adults, warfarin felt like a prison sentence - constant monitoring, dietary guilt, fear of interactions. Switching to a DOAC isn’t just medical - it’s liberating. But you’re right: adherence is everything. I’ve seen patients stop because they ‘felt fine’ - and then end up in the ER with a subdural. Set those alarms. Use the pill organizer. Even if you think you’re ‘good at remembering.’ You’re not. None of us are. And if you’re on dabigatran - keep it in the blister pack. Moisture is the silent killer. You got this.
Kimberly Mitchell
January 17, 2026Why are we pretending DOACs are magic? They’re just newer, more expensive blood thinners with fewer monitoring requirements because the manufacturers don’t want to pay for lab infrastructure. The reversal agents cost thousands and aren’t available in 80% of rural hospitals. Meanwhile, warfarin has been used safely for 70 years with a known reversal protocol. The real story here isn’t patient convenience - it’s corporate profit disguised as medical progress. Don’t be fooled.
Angel Molano
January 18, 2026Stop missing doses. You will bleed. You will die. This isn’t a suggestion. It’s physics.
Vinaypriy Wane
January 20, 2026I’ve been managing anticoagulation for over 15 years - in India, where access to labs and reversal agents is inconsistent. I’ve seen patients switch, and I’ve seen them suffer. The key isn’t just the INR or the CrCl - it’s the system. Do you have a pharmacist who calls you? A family member who knows the name of your drug? A card in your wallet? Without these, even the perfect dosing schedule fails. I tell my patients: ‘Your life is now a ritual - not a pill. It’s the alarm. The organizer. The follow-up. The conversation with your daughter about what to do if you fall.’ Technology helps - but humanity saves.
Randall Little
January 21, 2026So let me get this straight - we’re now recommending a class of drugs that require precise timing, have no universal reversal agents, demand renal monitoring, and are notoriously unforgiving of missed doses… because they’re ‘easier’ than a pill that’s been used since the Eisenhower administration? And we’re calling this ‘progress’? The irony is thick enough to spread on toast. Next up: replacing insulin with a ‘convenient’ glucose-mimicking spray that only works if you remember to take it at 8:03 a.m. and you haven’t eaten a cracker since yesterday. Brilliant. Just brilliant.