
Why Nighttime Medication Errors Happen
It’s 3 a.m. You’ve been on duty for 14 hours. Your eyes are heavy. The hospital is quiet. The only sounds are the beeping monitors and the hum of the air conditioner. You reach for a vial of insulin. The label is blurry. You double-check the dose. You’re sure it’s right. But you’re wrong. This isn’t a rare mistake. It’s a pattern.
Research shows that medication safety drops sharply during night shifts. A 2023 review of 38 global studies found that 82% of medication errors and near misses were linked to fatigue. Nurses, doctors, and pharmacists working overnight are more likely to misread labels, give the wrong dose, or skip critical steps-all because their brains are running on empty.
Your body isn’t designed to be awake at night. Circadian rhythms control everything from your body temperature to your alertness. When you fight that rhythm, your cognitive performance plummets. Studies show that after a single night without sleep, your ability to concentrate, remember details, and process numbers drops by 25-30%. That’s the same as having a blood alcohol level of 0.08%-legally drunk in most places.
Who’s Most at Risk
Nurses are hit hardest. They’re the ones handing out meds, checking names, verifying doses, and documenting everything-all while juggling multiple patients. A 2022 study across 15 U.S. hospitals found nurses working nights made 38% more medication errors than those on day shifts. The risk climbs even higher with overtime. Nurses working 12-hour shifts had a 15% higher error rate than those on 8-hour ones.
Doctors aren’t immune. Surgeons who got less than six hours of sleep had patients with 2.7 times more complications. Anesthesiologists who pulled an all-nighter showed a 23% drop in vigilance and an 18% drop in memory during simulated procedures. Emergency physicians on back-to-back night calls saw a 27% decline in visual memory and a 22% drop in overall thinking speed.
Even pharmacists aren’t safe. One study found that pharmacy technicians working overnight made more dosing errors when filling prescriptions for high-risk drugs like insulin, heparin, and opioids. These aren’t mistakes caused by carelessness. They’re caused by exhaustion.
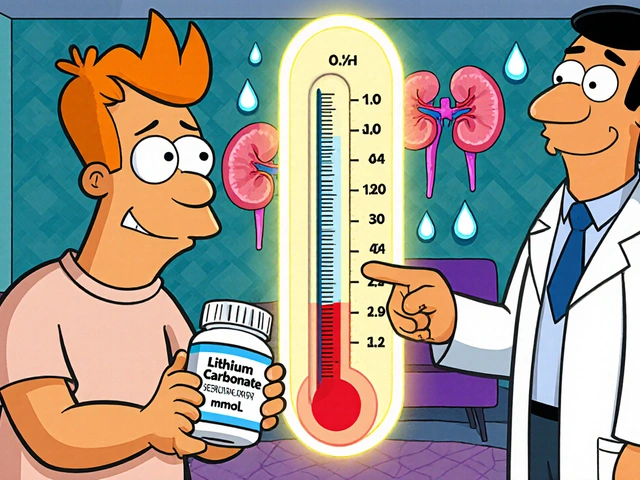
The Hidden Culprits: Medications That Make Fatigue Worse
Here’s something many healthcare workers don’t realize: the meds they take to cope with fatigue might be making it worse.
Antihistamines like diphenhydramine (Benadryl) are common sleep aids-but they cause drowsiness in 50-60% of users. Taking one before a night shift isn’t a fix. It’s a risk. Same with sleep pills like zolpidem (Ambien). Even though they’re meant to help you sleep, 15-20% of people still feel groggy the next day. Benzodiazepines like diazepam (Valium) leave residual sedation in 30% of users. Narcotic painkillers like oxycodone cause sedation in 25%. Even some antidepressants like trazodone make you feel like you’re moving through molasses.
The National Institute for Occupational Safety and Health (NIOSH) says: if you’re feeling overly sleepy at work, check your meds. Switching from diphenhydramine to loratadine (Claritin)-a non-sedating antihistamine-can cut your risk of error. Don’t assume your nighttime meds are harmless. They might be the silent cause of your mistakes.

What Actually Works: Proven Strategies to Stay Safe
There’s no magic bullet. But some strategies have real, measurable results.
System backups save lives. Automated alerts, barcode scanning, and double-check protocols reduce errors by 18%. A 2022 Johns Hopkins study showed that when hospitals used electronic double-checks for high-risk drugs, the number of mistakes dropped sharply. Don’t rely on memory. Use the system.
Caffeine helps-but only if timed right. A cup of coffee before your shift starts can boost alertness for 2-4 hours. But don’t chug it at 2 a.m. That’ll just mess up your sleep later. Stick to one or two cups early in the shift. Avoid sugar-laden energy drinks. They cause crashes that make you more vulnerable.
Napping isn’t lazy-it’s lifesaving. A 20-minute nap before a night shift can improve alertness by 12-15%. A 90-minute nap gives you a full sleep cycle, but you’ll feel groggy for 20-30 minutes after waking. That’s called sleep inertia. If you nap, plan for it. Don’t nap right before administering meds. Nap before your most critical tasks.
Breaks matter. Walking for five minutes every hour improves circulation and mental clarity. Stand up. Stretch. Look out a window. Even a short change of scenery resets your brain.
Why Work Hour Rules Haven’t Fixed This
In 2003, the Accreditation Council for Graduate Medical Education (ACGME) limited resident work hours to 80 per week. It sounded like a win. But the results? Mixed.
Some hospitals saw fewer errors. Others didn’t. Why? Because limiting hours doesn’t fix sleep deprivation if you’re still working nights. Many doctors can’t sleep during the day-noise, kids, anxiety, or just a racing mind. One night of total sleep loss takes three full days to recover from. And if you’re working three nights in a row? You’re running on a deficit you can’t repay.
Even worse, when shifts are shortened, handoffs increase. More transitions mean more chances for miscommunication. One study found that the number of errors during shift changes rose by 20% after work-hour limits were introduced.
The real solution isn’t just fewer hours. It’s better scheduling. More predictable shifts. Protected sleep time. And a culture that doesn’t shame people for saying, “I’m too tired to do this safely.”
What You Can Do Right Now
You don’t need to wait for policy changes. Start with these five steps tonight:
- Check your meds. Are you taking anything that makes you drowsy? Talk to your doctor about switching to non-sedating alternatives.
- Use tech. Scan barcodes. Use double-check systems. Don’t skip steps because you’re “in a rush.”
- Plan a nap. If you can, nap for 20 minutes before your shift. Even if you don’t sleep, lying down with eyes closed helps.
- Hydrate and move. Drink water. Walk every hour. Don’t sit still for long stretches.
- Speak up. If you’re too tired to think clearly, say so. Ask for help. It’s not weakness. It’s professionalism.
The Cost of a Single Mistake
Medication errors aren’t just statistics. They’re real people. A wrong dose of insulin can send someone into a coma. A misread antibiotic can trigger a deadly allergic reaction. These errors cost the U.S. healthcare system $20 billion a year. But the human cost? Priceless.
And it’s not just patients who suffer. Nurses and doctors who make errors often carry guilt for years. Some leave the profession. Others develop anxiety, depression, or PTSD.
This isn’t about blame. It’s about systems. Fatigue isn’t a personal failing. It’s a biological reality. When we ignore it, we put lives at risk.
Final Thought: Safety Isn’t Optional
You didn’t become a healthcare worker to hurt people. You didn’t train for years to make a mistake at 3 a.m. because you were too tired to read a label.
Medication safety at night isn’t about being perfect. It’s about building habits that protect you and your patients-even when your body is begging you to sleep. Use the tools. Speak up. Protect your rest. And remember: the most dangerous thing you can do is assume you’re fine.
Can caffeine replace sleep during night shifts?
No. Caffeine can temporarily boost alertness, but it doesn’t restore cognitive function lost from sleep deprivation. It masks fatigue without fixing it. Relying on caffeine long-term can disrupt your natural sleep cycle, making future shifts even harder. Use it as a short-term tool, not a solution.
Are night shift workers more likely to make medication errors than day shift workers?
Yes. Studies show medication errors are 12.1% more common during night or rotating shifts. Nurses on night shifts make 38% more errors than those on day shifts. Fatigue, circadian disruption, and reduced staffing all contribute to this increase.
What medications should night shift workers avoid?
Avoid sedating medications like diphenhydramine (Benadryl), zolpidem (Ambien), diazepam (Valium), oxycodone, and trazodone if you’re working nights. These can cause next-day drowsiness, impair judgment, and increase error risk. Ask your doctor for non-sedating alternatives like loratadine or melatonin (used correctly).
Is a 20-minute nap enough to improve performance?
Yes, for most people. A 20-minute nap can improve alertness by 12-15% and reduce errors in high-risk settings like ICUs and ERs. It avoids deep sleep, so there’s little to no sleep inertia. Longer naps (90 minutes) offer more rest but come with a 20-30 minute groggy period after waking-so plan accordingly.
Why don’t work hour limits prevent all medication errors?
Work hour limits reduce total hours but don’t fix sleep deprivation. Many workers still can’t sleep during the day due to noise, stress, or family demands. Also, shorter shifts mean more handoffs, which increase communication errors. Real change needs better scheduling, protected sleep time, and a culture that prioritizes rest over hustle.


Katherine Rodgers
December 4, 2025so u know what’s worse than being tired at 3am? realizing your benadryl is making you a walking zombie. i took it ‘for allergies’ and nearly gave a patient insulin instead of heparin. oops. my bad. 🙃
Lauren Dare
December 6, 2025The pharmacokinetic burden of sedating antihistamines in circadian-disrupted personnel is non-trivial. Loratadine, as a second-generation H1 antagonist, demonstrates negligible CNS penetration-thereby mitigating iatrogenic cognitive impairment. Why are we still prescribing diphenhydramine like it’s 1998?
Gilbert Lacasandile
December 7, 2025I really appreciate this post. I’ve been trying to nap before my night shift, but I always feel guilty about it. Like, ‘am I being lazy?’ But then I think-what’s more lazy: sleeping 20 minutes or screwing up a patient’s meds because I’m half-dead? Guess I’m choosing the nap now.
Lola Bchoudi
December 7, 2025System backups are non-negotiable. Barcode scanning + dual verification for high-alert meds reduces error rates by 18%-per JHMI 2022. If your facility doesn’t have this, advocate for it. Your brain is already compromised by circadian misalignment. Don’t let the system fail you too.
Morgan Tait
December 9, 2025You know what they don’t tell you? The hospital’s Wi-Fi is rigged. I swear, every time I scan a barcode at night, the system glitches. Coincidence? I think the pharmaceutical lobby is using subliminal signals to keep us groggy. They profit from mistakes. They profit from sleep deprivation. They profit from our silence.
Darcie Streeter-Oxland
December 10, 2025The notion that caffeine can serve as a viable substitute for sleep is not only scientifically fallacious, but also ethically indefensible within a professional healthcare context. The persistence of such myths reflects a systemic failure in medical education.
Taya Rtichsheva
December 10, 2025naps are cool and all but what about the fact that your alarm goes off at 5am after a 12 hour shift and you have to drive home? i once fell asleep at a red light and woke up to a horn blaring and a toddler in the backseat staring at me like i was the monster
Christian Landry
December 11, 2025i tried the 20-min nap before my shift and it was a game changer 🙌 even if i didn’t fall asleep, just closing my eyes for 15 mins felt like hitting reset. also switched from benadryl to claritin-no more zombie mode. my patients noticed. my boss noticed. i noticed. peace out, drowsiness 😴
Katie Harrison
December 13, 2025I appreciate the emphasis on systemic change, not individual blame. However, we must also acknowledge that institutional inertia-particularly in underfunded units-renders even the most evidence-based protocols unfeasible. Without adequate staffing, automation, and protected rest, these recommendations remain aspirational.
Mona Schmidt
December 14, 2025The data is clear: circadian misalignment impairs executive function equivalently to a BAC of 0.08%. Yet, we continue to normalize sleep deprivation as a badge of honor. This is not resilience. This is negligence. We owe our patients better. We owe ourselves better.
Guylaine Lapointe
December 14, 2025Let’s be honest-most of us are just too tired to care. We know the rules. We know the stats. We know the nap trick. But we’re too busy, too overworked, too afraid to say ‘I need help.’ And then we wonder why someone died from a wrong dose. It’s not a system failure. It’s a moral failure.
Sarah Gray
December 15, 2025I suppose it’s comforting to believe that fatigue is the real villain. Meanwhile, the real problem is that we’ve allowed unqualified, sleep-deprived individuals to handle life-altering medications. The solution isn’t naps-it’s hiring competent staff who don’t need caffeine to function.
Michael Robinson
December 17, 2025We’re all just meat machines trying to stay awake. The body doesn’t care about your schedule. It doesn’t care about your badge. It just wants to sleep. And when you fight it? You lose. Always.
Kathy Haverly
December 17, 2025Oh please. You think this is about fatigue? It’s about lazy nurses who don’t want to double-check. I’ve seen people scan barcodes but still give the wrong drug. The system works if you use it. Your tiredness is not an excuse-it’s a choice.
Andrea Petrov
December 19, 2025Have you ever considered that the whole ‘fatigue = error’ narrative is just a distraction? The real issue is that Big Pharma wants you to keep making mistakes so they can sell more meds to fix the complications. They own the hospitals. They own the guidelines. They own your sleep.
Suzanne Johnston
December 19, 2025There’s a quiet dignity in acknowledging one’s limits. To say, ‘I am not well enough to do this safely,’ is not weakness-it is the highest form of professional integrity. Yet, we punish those who speak up. We must change that culture.
Graham Abbas
December 21, 2025I remember one night-I was so tired I thought the insulin vial was saline. My hands were shaking. I didn’t know if I was holding the right thing. I walked out. I called my supervisor. I said, ‘I need a break.’ And guess what? No one yelled. No one fired me. They just said, ‘Thank you.’ That’s the kind of culture we need. Not more caffeine. More humanity.