
You’re sitting in the doctor’s office, counting the fading bruises on your arm from past blood draws, and you hear the words “lidocaine infusion.” Maybe your pain isn’t just an occasional visitor—maybe it’s been hijacking your days and nights for years, robbing you of quiet moments with your kids or even the joy of a walk around the block. When over-the-counter pills and physical therapy feel like jokes at your expense, you want more than hope. You want answers. Lidocaine infusions have become a buzz (sometimes literally) in pain clinics, with doctors offering this old-school anesthesia in a whole new way for people stuck in the nightmare of chronic pain. But does this treatment really deliver, or is it just another detour on the long road through pain management?
How Lidocaine Infusions Work, and Who Might Benefit
Lidocaine might seem like just another numbing shot at the dentist or ER, but as it turns out, this medication can do a lot more than kill surface pain. In an infusion, doctors deliver lidocaine directly into your bloodstream over a set period, usually around 30 minutes to a couple of hours, depending on the protocol. The whole idea is to quiet nerves that are stuck in overdrive—misfiring pain signals even when there’s no real physical threat. Think post-surgery nerve pain that won’t quit, fibromyalgia flare-ups so brutal they keep you hiding under blankets for days, or CRPS (complex regional pain syndrome)—that’s where lidocaine infusions sometimes step in.
Not every chronic pain is wired the same, though. Infusions work best for those whose pain is driven by nerve misfires. That means conditions like neuropathic pain, certain forms of headache, diabetic neuropathy, or pain syndromes with a strong nerve component. There’s some evidence for its use in intractable migraines, but don’t expect miracles if your pain comes from joint wear-and-tear or garden-variety arthritis. I remember a moment when Mae, my daughter, saw me getting frustrated about missing another family hike because of nerve pain in my legs. Sometimes, you just want options that haven’t failed you already.
The science here actually has a backbone. A 2023 meta-analysis in the journal Pain Medicine combed through 26 studies on lidocaine infusions in chronic pain and found that about 42% of patients reported "meaningful pain reduction"—that is, enough change to matter in daily life. That's not a lottery jackpot, but it's a big improvement compared to the 15% who get relief from a sugar-water placebo. In the same deep dive, side effects mostly ran mild: stuff like dizziness, numb lips, or a slightly spacey feeling. More serious side effects—such as irregular heartbeat or seizures—show up in less than 0.5% of cases, typically in people with risky heart rhythms or folks getting way too much lidocaine. Here's how it compares to other common pain relief options:
| Treatment | Avg. Response Rate | Primary Risks |
|---|---|---|
| Lidocaine infusion | 42% | Dizziness, mild sedation, rare cardiac issues |
| Opioid medications | 40-50% | Dependency, constipation, sedation |
| Physical therapy | 25-35% | Pain flares, muscle soreness |
| Anticonvulsants (e.g., gabapentin) | 30-40% | Fatigue, dizziness, mood changes |
It's pretty clear lidocaine infusion treatment finds its sweet spot in patients who can't tolerate pills, or those whose pain is sharper and more relentless than anything a Tylenol can fix. One Stanford pain doc, Dr. Sean Mackey, said it simply:
"Lidocaine infusions offer a middle ground for patients needing something more than pills but less drastic than nerve ablation. They're not a panacea, but they do have their place in the chronic pain toolbox."
To figure out if you’re a good candidate, providers usually run you through a screening gauntlet: ECGs to check for silent heart issues, a full medication review (lidocaine can interact with some antidepressants and anti-arrhythmics), and a quick look at your kidney and liver function. Age isn’t a deal-breaker, but your overall health and risk factors definitely play in. If you’ve got an allergic reaction history or epilepsy, you’ll want a detailed conversation before signing up. Usually, the pain clinic will start with a low test dose to see how you tolerate it before scheduling the real deal.
What to Expect During a Lidocaine Infusion: The Real Patient Experience
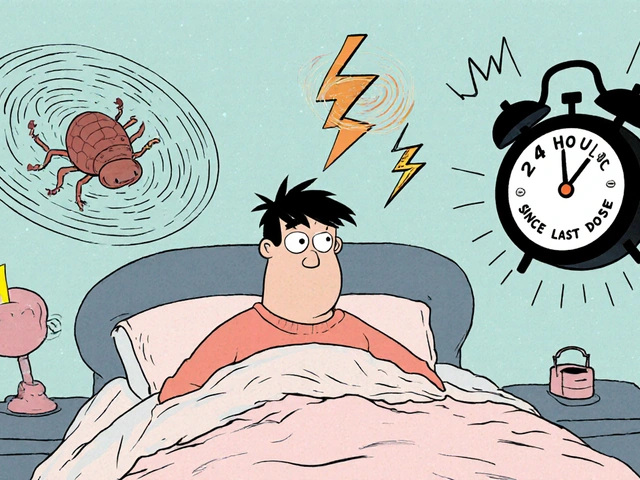
Let’s get real: getting a lidocaine infusion isn’t like popping an Advil or even getting a steroid shot. The setup usually means checking into an outpatient clinic or hospital setting. You won’t see any fancy sci-fi gear—just a recliner chair, maybe some warm blankets, and a nurse with pretty good IV skills. You show up in loose clothes (pro tip: short sleeves make everything easier), sign a stack of paperwork, and settle in. The IV goes into your arm or back of the hand, and you might notice a faint metallic taste or sudden tingling around your mouth not long after the drip gets going.
Nurses hover for the first 20 minutes, checking heart rate, blood pressure, and how well you’re handling the “buzz” feeling. Most people say the sensation is odd—not painful, just spacey, like sipping two strong espressos without the jitters. It can bring on a sense of weightlessness or, in rare cases, drowsiness. Occasionally, your tongue and lips go a bit numb. My buddy Jeff, who had persistent neuropathy after a work accident, joked that the first 10 minutes felt like floating in zero gravity, then he suddenly realized the throbbing pain in his foot was dialed down for the first time in two years.
Most infusions run between 30 and 120 minutes, depending on your size, diagnosis, and how you respond to the early test dose. The staff keeps tabs on your heart because lidocaine is, after all, a cardiac medication in its original life. Once the infusion wraps, you’ll chill for another half hour while the fog clears. Some patients feel woozy for an hour or two, so bring someone to drive you home—hospital policy won’t let you grab the bus solo.
- Bring a book, playlist, or show—it’s boring just staring at hospital tiles.
- Avoid caffeine before your appointment; lidocaine already amps up your nervous system a bit.
- If you’re anxious about needles, tell the nurse ahead of time. They almost always have numbing spray or distraction tricks.
- Plan for a lazy day: most people work from home or take the afternoon off after an infusion.
- Keep a symptom journal in the days after, noting changes in pain or side effects. This helps the doctor adjust dosing later.
So how soon do you get relief? That’s the wild card. Some folks walk out of the clinic feeling almost normal after years of agony. Others notice changes over the next 24 to 48 hours. The duration is unpredictable—anywhere from a few days to a few months. It usually takes two or three treatments before you really know if this therapy is going to work for you. And while it isn’t addictive, insurance coverage can be a mess: check ahead of time to avoid eye-popping bills down the road.
One of the most common frustrations is how long you might have to wait to see lasting results. Unlike opioid painkillers, which start working quickly, lidocaine’s pain-dampening effect can feel subtle or slow, sometimes requiring multiple sessions over weeks or even months. But when it hits, it tends to lower background pain enough to let people sleep better, move more, and participate in daily life. Some clinics recommend combining lidocaine infusions with physical therapy or counseling, because when pain ratchets down, other treatments finally have a shot at working.

Side Effects, Safety, and Practical Tips for Talking to Your Doctor
I won’t sugarcoat it—while lidocaine is considered safe in medical hands, things can go sideways if you have heart arrhythmias, take certain meds, or wind up with a rushed or under-trained provider. If you’ve ever passed out during an IV, be honest with your nurse—fainting is actually more common from nerves than any real lidocaine effect. Key short-term side effects include:
- Dizziness or light-headedness
- Mild confusion or "floaty" feeling
- Numbness or tingling around lips/tongue
- Occasional mild nausea
- Slight drop in blood pressure
More serious issues—fast heart rhythm changes, blurred vision, muscle twitches—show up very rarely, usually with high doses or in people with undetected cardiac vulnerabilities. If you’re allergic to amide-type anesthetics, this isn’t the treatment for you.
Now, the real sticky spot is that lidocaine infusions aren’t a cure—they’re a management tool, a way to dial pain down so you can get your life back. Consistency is key. Most protocols start with a "loading phase": one to three infusions spaced a week or two apart, then maintenance infusions every few months if results are good. If you only get one and toss the idea, you probably won't see the longer-term benefits.
Insurance coverage is hit or miss. Some plans cover lidocaine infusions when prior medications fail or side effects stack up. Others consider it experimental for off-label uses (think fibromyalgia, post-herpetic neuralgia). Always have your clinic run a benefits check before scheduling—one surprise bill is all it takes to sour the experience.
Talking to your doctor about lidocaine infusion therapy? Come armed with questions. Here are a few that get straight to the point:
- "What types of chronic pain respond best to lidocaine infusions?"
- "How will you monitor me for side effects during and after the infusion?"
- "How many treatments, on average, will I need before noticing results?"
- "Will you coordinate with my current pain management team?"
- "What’s my out-of-pocket cost after insurance? Any financial support available?"
You’re not being a pest by asking for details. In 2022, the American Society of Regional Anesthesia reported that patient engagement—meaning, people who ask tough questions—improves pain control and treatment satisfaction. Don’t let anyone rush you if you’re uneasy.
And a last tip? Connect with others who’ve had this done (support forums or in-person groups). There’s a lot you can learn from the real-life stories—not just medical stats. I’ve found people are surprisingly generous sharing what infusion days feel like, how they manage anxiety, and whether the cost and hassle are worth the “off switch” on relentless pain.
For families navigating this with kids or teens, know that pediatric protocols exist, but doses are much more cautious. Some studies even suggest cautious lidocaine infusion therapy can help younger patients with severe nerve pain when other approaches flop. Always check if your doctor has hands-on experience with children or younger adults, though—kids aren’t just small adults.
If chronic pain is clogging up your days, and you’re juggling endless doctor visits, this isn’t some miracle solution, but it might be the break you need to reclaim a bit of yourself. Lidocaine infusions ask for patience, a bit of faith, and the guts to try something new when nothing else is working. Sometimes, that’s exactly what stubborn pain—the kind that doesn’t respect weekends or birthdays—requires. And no, you’re not weak for needing help; you’re just fighting to get back your life.


Kelly McDonald
May 19, 2025Lidocaine infusions felt like a lifeline when nothing else worked-my fibro pain was a constant scream, and this? It turned the volume down to a whisper. I didn’t believe it at first, but after the third session, I slept through the night for the first time in years. No opioids. No crashes. Just quiet. I still get infusions every six weeks. Worth every penny, every minute.
And yes, the tingling lips are weird. But so is living in pain that doesn’t care if it’s your birthday.
harvey karlin
May 20, 2025Neuropathic pain = NMDA receptor chaos. Lidocaine’s a sodium channel blocker-hits the hyperexcitable neurons like a reset button. Not magic, just neuropharmacology. Works best when the pain’s peripheral, not central. If your pain’s all in your head? This won’t fix it. But if it’s your nerves screaming? Yeah. Game-changer.
Pro tip: Pair with low-dose naltrexone. Synergy.
Anil Bhadshah
May 22, 2025I work in a pain clinic in Delhi. We’ve done over 200 lidocaine infusions. Success rate? Around 40-45%. Most patients are elderly with diabetic neuropathy. Side effects? Rare. But we always check ECG first. One guy had a fainting spell-turned out he hadn’t eaten. Simple fix.
Always tell patients: this isn’t a cure. It’s a pause button. Use it to rebuild.
Also, insurance here doesn’t cover it. Pay out-of-pocket. But if you can afford it? Do it.
Trupti B
May 24, 2025i did one of these last month and it was kinda wild like my tongue went numb and i felt like i was floating but the pain in my foot just... stopped like someone flipped a switch idk if itll last but for now im just glad to walk without crying
Joe Gates
May 24, 2025You know, I used to think chronic pain was just something you had to endure-like bad weather you couldn’t escape. But then I saw someone who’d been bedridden for five years get up after their third infusion and hug their grandkid without wincing. That’s not medicine. That’s a miracle with a drip line.
It’s not about the drug. It’s about the moment your body remembers what it’s like to be free. And that? That’s worth every awkward tingling lip, every hour spent in a recliner, every insurance battle. You’re not broken. You’re just waiting for the right key.
And if you’re scared? Good. That means you still care. And if you still care, you still have a shot.
I’m not saying this will work for everyone. But I’m saying: try it. Not because it’s trendy. But because you deserve to feel the sun on your skin without pain stealing the moment.
Tejas Manohar
May 25, 2025As a board-certified pain specialist, I must emphasize that lidocaine infusions are an off-label intervention for most chronic pain conditions. While the evidence base is growing, particularly for neuropathic syndromes, it remains a second- or third-line option. Rigorous patient selection is paramount.
Contraindications include known hypersensitivity to amide anesthetics, second- or third-degree heart block without a pacemaker, and severe hepatic impairment. Pre-infusion cardiac monitoring is non-negotiable.
Patients must be counseled that this is not a cure, nor a substitute for multidisciplinary care. Integration with physical rehabilitation and psychological support remains essential for sustained outcomes.
Do not pursue this treatment without a comprehensive pain assessment and documented failure of at least two first-line pharmacologic modalities.
VEER Design
May 25, 2025Man, I tried this after 7 years of CRPS. First infusion? Felt like my leg was underwater. Second? I walked to the mailbox without limping. Third? I danced with my wife at our anniversary dinner. No joke.
But here’s the thing-don’t expect the clinic to hold your hand. They’ll give you the drip. The rest? You gotta do the work. PT. Journaling. Sleep hygiene. This isn’t a magic wand. It’s a spark. You gotta fan the flame.
Also, bring headphones. The silence in that room? Heavy. Music saved my sanity.
And yeah, I cried after the first one. Not from pain. From relief. You don’t know how loud silence can be until you’ve lived with screaming nerves for years.
lili riduan
May 27, 2025I’m a mom of two, and I used to cry in the shower because standing to brush my teeth hurt too much. After my third lidocaine infusion, I picked up my toddler without thinking. Just... picked him up. And he laughed. And I didn’t cry.
That’s the moment I realized: this isn’t about pain. It’s about being present. About being the person your kids need.
It’s not perfect. I still have bad days. But now? I have tools. I have hope. And I have a little more time with them.
Don’t let fear of needles or insurance nightmares steal that from you. Ask. Push. Advocate. You’re worth the fight.
Jensen Leong
May 29, 2025It’s interesting how medicine often reduces human suffering to statistical efficacy. 42% response rate. But what does that mean for the individual who is the 42%? It means the difference between watching your child’s soccer game from the sidelines and being on the field, cheering with your whole body.
The body remembers trauma. Not just the injury, but the years of being told it’s "all in your head." Lidocaine doesn’t erase the past-it gives the nervous system a chance to forget how to scream.
This isn’t about drugs. It’s about dignity. And if we’re going to call ourselves healers, we must offer more than pills and platitudes. We must offer moments. Even fleeting ones. Especially the fleeting ones.
Mohd Haroon
May 31, 2025The Western medical paradigm has long dismissed neuropathic pain as psychosomatic or resistant. This bias has delayed effective interventions for decades. Lidocaine infusion, though underutilized, is a scientifically grounded modality that challenges the reductionist model of pain as merely tissue damage.
Neuroplasticity is not a buzzword-it is a physiological reality. Lidocaine, by transiently silencing aberrant nociceptive signaling, allows the central nervous system to recalibrate. This is not placebo. This is neurophysiology.
That said, access remains inequitable. In developing nations, cost and infrastructure limit availability. We must advocate not just for clinical adoption, but for equitable distribution. Pain does not discriminate. Neither should care.