
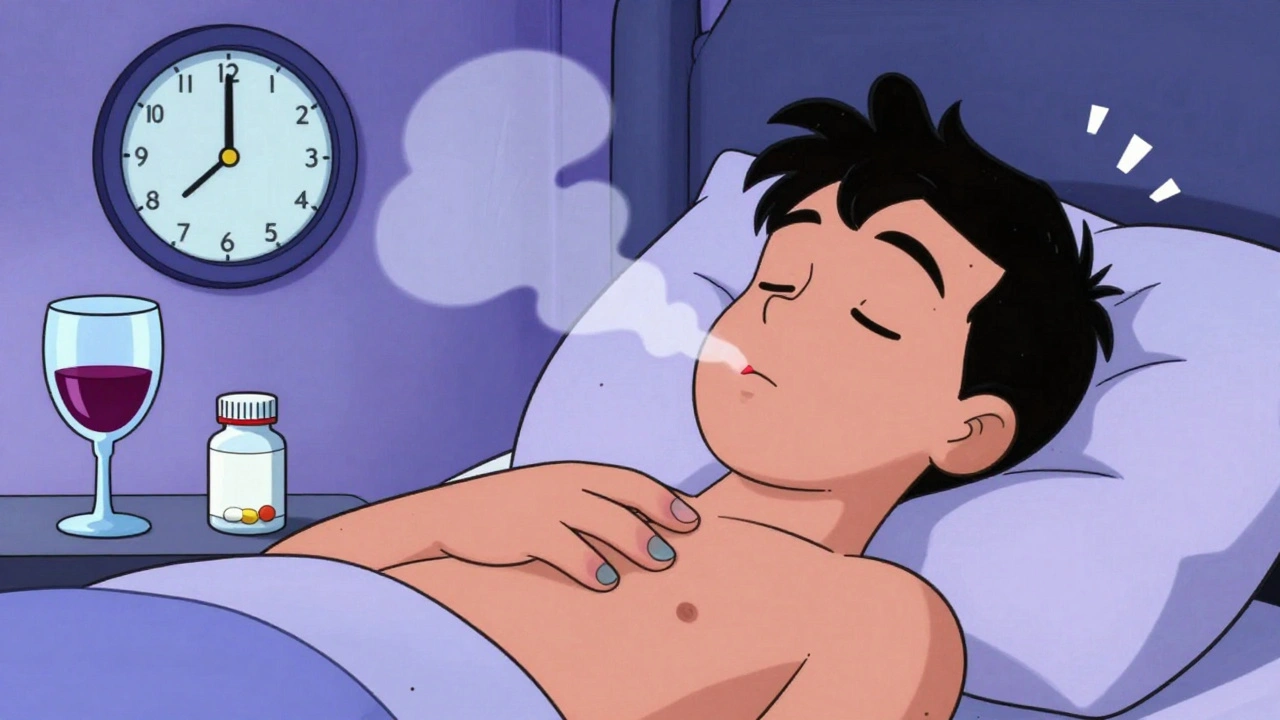
Someone you care about takes a pill to sleep. They’re quiet. Too quiet. Their breathing is slow. Their lips are turning blue. You shake them. No response. This isn’t just deep sleep. This is an overdose-and every minute counts.
What Counts as a Sedative Overdose?
Sedatives and sleep medications slow down your brain and nervous system. That’s how they help you relax or fall asleep. But when too much builds up in your body, they don’t just make you sleepy-they shut down your breathing. This isn’t rare. In 2021, over 12,500 people in the U.S. died from overdoses involving benzodiazepines like Xanax or sleep drugs like Ambien. That’s more than double the number from 2010. These drugs include prescription benzodiazepines (diazepam, alprazolam, temazepam), "Z-drugs" (zolpidem, eszopiclone), barbiturates, and even some over-the-counter sleep aids like Tylenol PM, which contains diphenhydramine. Even melatonin, often seen as harmless, can cause dizziness and nausea at very high doses-but it doesn’t stop your breathing. That’s the key difference. Prescription sedatives can.The Warning Signs: What to Look For
Recognizing an overdose isn’t about guessing. It’s about spotting clear, physical changes. Here’s what to watch for, in order of progression:- Unresponsiveness: Can you wake them up? Shout their name. Shake their shoulder. Try a sternal rub (rub your knuckles hard on the center of their chest). If they don’t react at all, it’s not sleep. It’s danger.
- Slurred speech: Words come out thick, slow, or jumbled. This happens in 87% of benzodiazepine overdoses.
- Extreme drowsiness: Not just tired. Not just groggy. They can’t keep their eyes open, even when you’re yelling. They slump like a ragdoll.
- Slow, shallow breathing: Count their breaths for 30 seconds. If they take fewer than 6 breaths in that time (less than 12 per minute), they’re in respiratory failure. Normal is 12-20. Below 8? They’re minutes from stopping breathing entirely.
- Cyanosis: Lips, fingertips, or nails turn blue or gray. This means their blood isn’t getting enough oxygen.
- Cold, clammy skin: Their body temperature drops. Skin feels wet and icy. This signals their system is shutting down.
- Loss of coordination: They can’t stand, walk, or hold their head up. Movements are clumsy, like they’re drunk-but they haven’t had alcohol.
- Vomiting: Especially if they’re unconscious. This can lead to choking.
- Coma: If they’re completely unresponsive and their Glasgow Coma Scale score drops below 8, they’re in a medical coma. Survival depends on immediate help.
Not All Overdoses Look the Same
Different drugs cause different symptoms. Mixing them makes it worse.- Benzodiazepines (Xanax, Valium, Ambien): Often cause deep sedation with surprisingly stable heart rate and blood pressure-until they don’t. Respiratory failure hits fast. Many people think they’re just "passed out" because their pulse is still there.
- Barbiturates (phenobarbital): Rarely prescribed now, but still deadly. They depress breathing at lower doses than benzodiazepines. Fatality rates are higher.
- Over-the-counter sleep aids (diphenhydramine): Can cause hallucinations, seizures, rapid heartbeat, and urinary retention. These aren’t typical of prescription sedatives. But they’re still dangerous.
- Combination overdoses: Mixing sedatives with alcohol or opioids is the deadliest combo. The CDC found that 23% of benzodiazepine deaths in 2021 also involved fentanyl. Alcohol multiplies the depression effect. One pill plus one drink can be enough.
What You Must Do Immediately
If you see any of these signs, don’t wait. Don’t hope they’ll wake up. Don’t try to make them vomit or give them coffee. Here’s what works:- Call emergency services right now. Say: "Someone overdosed on sleep medication. They’re not waking up and their breathing is slow." Every minute lowers survival chances by 7-10%.
- Check breathing. If they’re not breathing or taking fewer than one breath every 5 seconds, start rescue breathing. Tilt their head back, pinch their nose, give one breath every 5 seconds. Don’t stop until help arrives.
- Don’t give flumazenil. This is the only antidote for benzodiazepines, but it can trigger seizures in people who are dependent on these drugs. Only trained medical staff should use it.
- Stay with them. Keep them on their side if they’re unconscious. This prevents choking if they vomit.
- Bring the medication bottle. Emergency responders need to know exactly what was taken. Empty pill containers, prescription labels, or even text messages about dosage can help.
Why People Delay Calling for Help
A 2022 study found that 68% of bystanders didn’t realize what they were seeing was an overdose. They thought the person was just "really tired," "drunk," or "sleeping it off." One Reddit user wrote: "I thought my roommate was just exhausted from work." Another said: "I assumed the slurred speech was from drinking." But here’s the truth: sedative overdose doesn’t come with a warning label. It creeps in. The person might have taken their normal dose. Or maybe they took an extra pill because they couldn’t sleep. Or they drank a glass of wine with it. The line between "safe" and "deadly" is thin-and invisible until it’s too late.
Who’s at Highest Risk?
- Adults aged 25-54: This group saw the steepest rise in overdose deaths between 2010 and 2021. - People with multiple prescriptions: Taking sedatives from different doctors without telling them increases overdose risk. - Those with mental health conditions: Anxiety, depression, and PTSD are linked to higher sedative use and misuse. - People who use sedatives long-term: Tolerance builds. They take more. The risk of accidental overdose rises. - Those using with alcohol or opioids: This combo is responsible for most fatal cases.What’s Being Done to Stop This?
New tools are emerging. In 2023, the FDA approved intranasal midazolam for emergency use. Some hospitals now use continuous pulse oximeters that monitor oxygen levels overnight-catching drops before breathing stops. California distributed 250,000 overdose recognition cards to pharmacies. Early results show a 22% increase in bystander action. But the most powerful tool is still you. Knowing the signs. Acting fast. Not waiting for someone to "wake up on their own."Prevention Starts with Awareness
If you or someone you know takes sedatives:- Never mix them with alcohol or opioids.
- Take exactly as prescribed. No extra pills, even if you didn’t sleep well.
- Keep medications locked up. Especially if teens or others live in the house.
- Ask your doctor: "Is this the safest option for me?" Many sleep issues can be managed with therapy or lifestyle changes.
- Know your local poison control number. Save it in your phone.
Most sedative overdoses happen at home. In bedrooms. On couches. Behind closed doors. There’s no siren. No alarm. Just silence. And slow breathing. If you recognize it, you can save a life.
Can you overdose on melatonin?
Yes, you can take too much melatonin, but it’s not life-threatening like prescription sedatives. Doses as high as 240mg (60 times the normal amount) have been reported, causing only headaches, dizziness, nausea, or vivid dreams. Unlike benzodiazepines or Z-drugs, melatonin doesn’t suppress breathing or cause coma. It’s not a sedative in the medical sense-it’s a hormone that helps regulate sleep cycles.
Is flumazenil safe to use at home?
No. Flumazenil is the only antidote for benzodiazepine overdose, but it’s extremely dangerous outside a hospital. It can trigger sudden seizures in people who are physically dependent on these drugs. The FDA has documented 17 fatal seizures from improper use. Only trained medical staff should administer it. Never try to get or use it yourself.
Can someone recover from a sedative overdose without treatment?
It’s possible, but extremely risky. Many people who survive without help suffer brain damage from lack of oxygen. Others slip into a coma and die hours later. Even if they wake up, the body may still be absorbing the drug. Medical monitoring is essential. Recovery isn’t just about waking up-it’s about making sure the drug is fully cleared and no secondary complications occur.
What’s the difference between sedative and opioid overdose?
The classic signs of opioid overdose are pinpoint pupils, blue lips, and very slow breathing. Sedative overdose often looks similar, but pupils are usually normal-sized, not pinpoint. However, in mixed overdoses-like benzodiazepines plus fentanyl-the signs blur. That’s why you should never assume you know the cause. If someone is unresponsive and breathing poorly, treat it as an emergency regardless of the drug.
How long does it take for a sedative overdose to become fatal?
It can happen in under 30 minutes, especially with barbiturates or when mixed with alcohol. In benzodiazepine-only cases, it may take longer-up to a few hours-but respiratory depression can quietly worsen. The longer you wait, the higher the chance of brain injury or death. Emergency responders say the first 10 minutes are critical. Calling 911 immediately is the only reliable way to prevent fatality.




Harriet Wollaston
December 13, 2025My sister took Xanax for years after her accident. I never realized how dangerous it was until she almost didn’t wake up one night. I thought she was just sleeping it off. This post? It saved my life. I keep the warning signs printed on my fridge now. If you take these meds, please, please, please tell someone you trust. Don’t suffer in silence.
And if you’re reading this and you’re scared to ask for help? You’re not weak. You’re human. And you deserve to be safe.
I’m so glad this exists.
Lauren Scrima
December 14, 2025So… you’re telling me that if someone’s breathing like a sloth on sedatives, you shouldn’t just shake them and yell ‘wake up’? Shocking. Who knew?
Also, melatonin isn’t a sedative? Wow. I thought it was just magic sleep fairy dust. Thanks for clearing that up. 🙄
Hamza Laassili
December 15, 2025Yall need to stop being so soft. People take too many pills? That’s what happens when you let the weak survive. I got a cousin who OD’d on Ambien-he was lazy, didn’t work, drank too much. He deserved what he got. Emergency services? Nah. Let ‘em sleep it off. The gene pool gets cleaner that way.
Also, why are we even talking about this? Just lock up the pills. Problem solved. No more whining.
Rawlson King
December 15, 2025The real issue isn’t the drugs-it’s the cultural collapse that normalizes chemical escapism. People no longer tolerate discomfort. They don’t meditate. They don’t journal. They don’t sit in silence with their thoughts. Instead, they reach for a pill like it’s a goddamn pacifier. This isn’t a medical crisis. It’s a spiritual failure.
And yes, I’ve seen this in three countries. You’re not ready for the truth.
Also, flumazenil is a band-aid on a severed artery. Stop treating symptoms. Treat the soul.
Constantine Vigderman
December 17, 2025OMG THIS IS SO IMPORTANT!! I just shared this with my whole family!! My aunt takes Ambien and she’s 68 and I was so scared for her!! Now I know what to look for!! I printed out the warning signs and taped them to her medicine cabinet!! I even made a little chart with emojis!! 😇💤🚨
Also, if you’re reading this and you’re taking meds, PLEASE talk to your doctor!! I did and she switched me to a natural sleep routine!! I’m sleeping better than ever!! 🙌✨
PS: I saved poison control in my phone!! I’m literally a hero now!!
Cole Newman
December 17, 2025Bro, I’ve been taking 3 zolpidem pills a night for 5 years. I’m fine. I don’t even feel it anymore. You think I’m gonna stop because some blog says I might die? Nah. I’ve got a job, a kid, and a dog. I’m not a junkie. I’m just tired. And if you’re gonna judge me for sleeping, you can go cry into your kale smoothie.
Also, your ‘sternal rub’ thing? That’s assault. I’d call the cops if someone did that to me.
Emily Haworth
December 19, 2025Did you know the FDA is secretly testing sedatives in the water supply? They’re trying to make us docile so we don’t protest. That’s why they downplay melatonin. It’s a cover-up. They don’t want you to know that the real danger is the government’s chemical mind control program. I’ve got a friend who works at a pharmacy. She says the pills are labeled wrong on purpose. They want you to OD so they can track your DNA.
Also, why is there no mention of 5G? I think the radiation makes the drugs more potent. I’m not crazy. I’ve read the docs.
Send help. Or don’t. They’re watching anyway. 👁️
Yatendra S
December 19, 2025Life is a series of chemical negotiations between the self and the void. Sedatives are merely mirrors of our collective existential fatigue. We do not overdose on pills-we overdose on meaninglessness. The blue lips? They are the color of silence after the last prayer. The slow breath? It is the rhythm of a civilization forgetting how to feel.
Flumazenil cannot heal the wound of modern alienation. Only stillness can. But stillness requires courage. And courage, like sleep, is now a luxury.
So we take the pill. And we wait. And we hope the silence is gentle.
Himmat Singh
December 21, 2025It is, with profound regret, incumbent upon me to observe that the proliferation of such content, while ostensibly well-intentioned, inadvertently fosters a culture of pathological dependency and medical infantilization. The notion that an individual requires external intervention to manage the natural exigencies of sleep is, in my estimation, emblematic of a broader societal decline in personal responsibility. Furthermore, the inclusion of anecdotal testimonies in lieu of peer-reviewed longitudinal data undermines the integrity of public health discourse. One is compelled to ask: if the solution is merely to ‘call 911,’ then what, pray tell, is the role of self-discipline? Or, indeed, of the human will?
kevin moranga
December 21, 2025Hey, I just want to say thank you for writing this. I’ve been a nurse for 18 years and I’ve seen too many people lose their lives because someone thought they were just ‘passed out.’ I’ve had families come in crying because they didn’t know the difference between sleep and overdose. This post? It’s the kind of thing that saves lives.
My niece took 10 melatonin gummies once because she thought it was candy. She threw up for 12 hours and was so scared. But she woke up. No brain damage. No hospital. That’s the difference.
But if someone takes a Xanax and a glass of wine? That’s a death sentence waiting to happen. I’ve seen it. I’ve held their hand while they stopped breathing.
So please-don’t wait. If you see someone not waking up, call 911. Don’t wait for them to ‘get better.’ Don’t wait for someone else to act. You’re the one who’s there. You’re the one who can save them.
And if you’re taking these meds? Talk to your doctor. Ask if there’s another way. You’re not broken. You’re just tired. And that’s okay. But you don’t have to do it alone.
Alvin Montanez
December 23, 2025Let me be perfectly clear: this entire post is a dangerous, emotionally manipulative piece of performative activism disguised as public service. You are not helping people by encouraging them to call 911 every time someone looks sleepy. You are creating a generation of codependent, fear-driven individuals who believe their only duty is to react-not to think, to grow, to endure. The fact that you equate taking a prescribed medication with moral failure is abhorrent. People are not victims of pharmacology-they are agents of their own choices. If someone overdoses, it is not because society failed them. It is because they failed themselves.
And let’s not pretend melatonin is harmless. It’s a hormone. Manipulating circadian rhythms without medical supervision is reckless. You’re not protecting people-you’re enabling them to avoid accountability. Real compassion is teaching someone to sleep without pills, not handing them a pamphlet and calling it a day.
Also, the CDC statistics you cite? They’re cherry-picked. The rise in benzodiazepine deaths correlates directly with the opioid epidemic and the overprescribing of fentanyl. Blaming sedatives is like blaming the flashlight for a car crash.
Stop treating people like children. Teach them discipline. Teach them resilience. Teach them to live with discomfort. That’s the only antidote worth having.