
Starting a new medication can feel overwhelming. You’re handed a pill bottle, a prescription slip, and maybe a quick explanation from a doctor who’s running late. But here’s the truth: medication safety isn’t just about taking your pills-it’s about understanding how, when, and why you take them. For first-time patients, getting this right can mean the difference between feeling better and ending up in the emergency room.
In the U.S. alone, over 1.3 million people visit the ER each year because of bad reactions to medications. Many of these cases aren’t accidents-they’re preventable. The good news? Simple, consistent habits can cut your risk of harm by up to half. You don’t need to be a doctor. You just need to know what to ask, what to watch for, and how to stay organized.
Know the Six Rights of Medication Use
Healthcare professionals use a checklist called the Six Rights to avoid mistakes. As a patient, you should use it too. These aren’t just hospital rules-they’re your personal safety net.
- Right patient: Make sure the name on the bottle matches yours. Double-check your date of birth if you’re picking up meds at the pharmacy.
- Right medication: Compare the pill you’re holding to the prescription. If it looks different from last time, ask why. Generic versions are safe, but they often look different.
- Right indication: Ask your doctor or pharmacist: "What is this medicine for?" Don’t assume. A pill meant for high blood pressure might be mistaken for something else.
- Right dose: Never use kitchen spoons. A teaspoon from your drawer can be 25% more or less than the correct amount. Use the measuring cup or syringe that came with the medicine.
- Right route: Is it meant to be swallowed, placed under the tongue, applied to the skin, or injected? Taking a patch orally or injecting a pill can be dangerous.
- Right time: Some meds need to be taken with food. Others must be taken on an empty stomach. Some work better in the morning; others at night. Ask when and why.
Write these six points on a sticky note. Keep it next to your pill organizer. You’ll thank yourself later.
Keep a Complete Medication List
Most people don’t realize they’re taking more than they think. Prescription drugs? Check. Over-the-counter painkillers? Check. Vitamins, herbal supplements, even CBD oil? Those count too.
A 2022 study found that patients who kept a full list of everything they took had 27% fewer medication errors. That’s not a small number-it’s life-changing.
Here’s what to include:
- Drug name (brand and generic if different)
- Dose (e.g., 10 mg, 500 mg)
- How often (e.g., once daily, every 8 hours)
- Why you’re taking it (e.g., "for high blood pressure", "for joint pain")
- When you started
- Pharmacy name and number
Keep this list on your phone and in your wallet. Bring it to every appointment-even if you think nothing changed. Doctors miss things. Pharmacists don’t always know what you’re taking unless you tell them.
Never Take Someone Else’s Medicine
"My friend said this helped their headache. Can I try it?"
No. Never.
The FDA says sharing medications causes about 8% of emergency visits for drug reactions. Why? Because what works for one person can harm another. A pill that lowers blood pressure for your aunt might crash your heart rate. Antibiotics prescribed for a sinus infection won’t help your toothache-and could make your body resistant to real treatments later.
Even if it’s "just one pill," it’s not worth the risk. If you’re in pain or feeling unwell, call your doctor. Don’t borrow.
Store Medications Properly
Your meds aren’t meant to sit in the bathroom cabinet. Heat, moisture, and light can break them down-sometimes without you noticing.
Here’s what you need to know:
- Insulin: Must be refrigerated (36-46°F) until first use. After opening, it can stay at room temperature for up to 28 days.
- Most pills: Keep in a cool, dry place-like a bedroom drawer. Avoid the bathroom or kitchen near the stove.
- Liquid medicines: Some need refrigeration. Check the label.
- Controlled substances (like opioids or strong anxiety meds): Lock them up. These can be dangerous if someone else finds them.
Expired meds? Toss them. The FDA says 18% of medication errors come from using drugs past their expiration date-especially antibiotics and liquid forms. They lose strength or turn toxic. Don’t risk it.

Read the Label Like a Pro
Pharmacy labels are small. The print is tiny. You’re tired. You’re in a rush. But reading the label in good light isn’t optional-it’s essential.
15% of medication errors happen because people misread labels. That’s like flipping a coin every time you take a pill.
Here’s how to read it right:
- Turn on a bright light.
- Use reading glasses if you need them.
- Check the drug name, dose, and instructions.
- Look for warnings: "Avoid alcohol," "May cause drowsiness," "Take on empty stomach."
- Check the expiration date.
If you can’t read it clearly, call the pharmacy. They’ll print a larger label or explain it over the phone. No shame in asking.
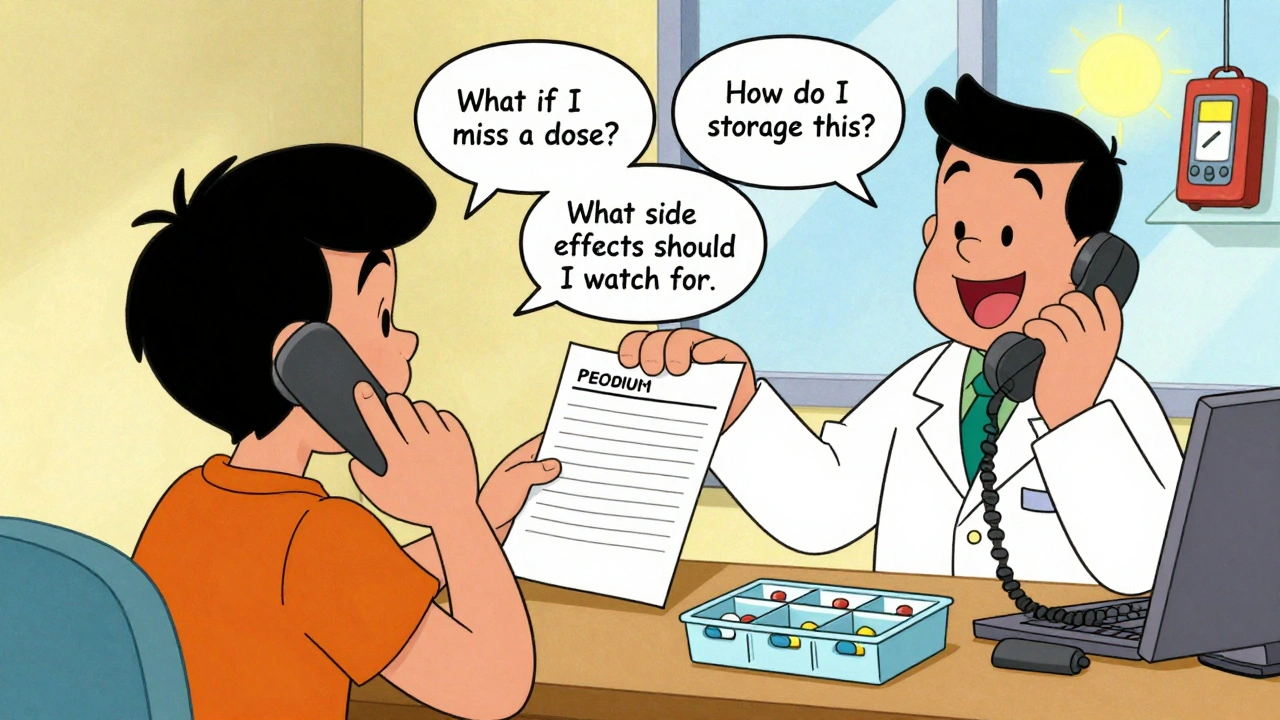
Ask Questions-Even If They Feel Stupid
Most patients don’t ask enough questions. A 2022 study showed that people who asked three or more questions about a new medication had 34% fewer side effects in the first month.
Here are the three questions you must ask every time you get a new prescription:
- "What should I do if I miss a dose?" Only 22% of patients ask this. The answer matters. Some meds you skip. Others you double up. Some you call your doctor about.
- "How should I store this?" Forty percent of medications need specific conditions. If you don’t know, you might ruin the drug before you even take it.
- "What side effects should I watch for?" Only 65% of pharmacy visits cover this. You need to know what’s normal (like mild nausea) and what’s dangerous (like swelling, chest pain, or trouble breathing).
Write these questions down. Bring them to your appointment. Don’t leave without answers.
Use Tools to Stay on Track
Forgetfulness is the #1 reason people don’t take meds right. It’s not laziness-it’s human.
Apps like Medisafe and MyMeds help. They send reminders, track doses, and even scan your pill bottle to confirm you’re taking the right one. A 2022 study found they improved adherence by 28% in first-time users.
Not into apps? Try these low-tech fixes:
- Use a pill organizer with days and times labeled.
- Set phone alarms for each dose.
- Pair taking meds with a daily habit: after brushing your teeth, with breakfast, before bed.
One patient in Melbourne started using a kitchen timer to remind herself to take her blood thinner. She hadn’t missed a dose in 11 months.
Watch for Changes and Speak Up
Generic drugs are safe and save money. But they often look different from the brand name version. A pill that was blue might now be white. The shape might change. The imprint might be different.
That doesn’t mean it’s wrong. But it does mean you should ask: "Is this the same medicine?"
90% of prescriptions in the U.S. are filled with generics. Pharmacists switch them automatically unless your doctor says "dispense as written." Don’t assume it’s a mistake. But don’t assume it’s identical either. Ask.
Also, if you start feeling strange-dizzy, nauseous, itchy, confused-don’t wait. Call your pharmacist. They’re trained to spot drug reactions. They can tell you if it’s normal or if you need to see a doctor right away.
Be Careful During Transitions
The biggest spike in medication errors happens when you leave the hospital.
22% of mistakes occur during discharge. You get a new list of meds, maybe a few changes, and are sent home with instructions you barely understood.
Before you leave:
- Ask for a written discharge summary with all your meds listed.
- Compare it to your own list. Are there new ones? Removed ones?
- Ask: "What’s different now? Why?"
- Call your regular doctor within 48 hours to review the changes.
Don’t wait for a follow-up appointment. Act fast.
It Gets Easier-But Stay Vigilant
Learning to manage meds safely takes time. Most people need 2 to 3 weeks to build the routine. It’s not about memorizing everything. It’s about building habits: checking labels, keeping a list, asking questions, using reminders.
The goal isn’t perfection. It’s awareness. You don’t have to be an expert. You just have to care enough to ask, check, and speak up.
Medication safety isn’t a one-time task. It’s a lifelong habit. And the better you get at it, the safer you’ll be.
What should I do if I accidentally take the wrong dose?
Don’t panic, but act quickly. Call your pharmacist or poison control immediately (1-800-222-1222 in the U.S.). Do not wait for symptoms. Tell them exactly what you took, how much, and when. If you’re feeling unwell-like dizziness, vomiting, or chest pain-go to the ER. Never try to "make up" for a missed or extra dose by doubling the next one unless instructed by a professional.
Can I crush or split my pills?
Only if your doctor or pharmacist says it’s safe. Some pills are designed to release medicine slowly over time. Crushing them can cause too much drug to enter your system at once. Others have coatings to protect your stomach or make them easier to swallow. Always ask before altering your medication. If swallowing is hard, ask for a liquid version instead.
Are herbal supplements safe with prescription drugs?
Not always. Supplements like St. John’s Wort, garlic, ginkgo, and even high-dose vitamin E can interfere with blood thinners, antidepressants, and heart medications. Many people assume "natural" means safe, but that’s not true. Always tell your pharmacist about every supplement you take-even if you think it’s harmless.
Why do I get different-looking pills from the same pharmacy?
It’s likely a switch to a different generic manufacturer. Pharmacies often choose the lowest-cost option available. Generic drugs have the same active ingredient and work the same way, but they can look different in color, shape, or imprint. Always check the name and dose on the label. If you’re unsure, ask the pharmacist to confirm it’s the same medication.
How do I know if a medication is expired?
Check the expiration date printed on the bottle or box. It’s usually labeled "EXP" followed by a month and year. For example, EXP 06/2026 means it’s good until the end of June 2026. If the pill is discolored, smells odd, or has changed texture (like becoming crumbly or sticky), throw it out-even if the date hasn’t passed. Liquid medicines and insulin are especially sensitive to time and temperature.
Can I drink alcohol while taking my medication?
It depends. Alcohol can make some meds too strong-like sedatives, painkillers, or anxiety drugs-and cause dangerous drowsiness. With others, like antibiotics or blood pressure pills, it can reduce effectiveness or increase side effects like nausea or dizziness. Always check the label for warnings. If it’s not clear, ask your pharmacist. When in doubt, skip the alcohol.
Next Steps: Build Your Safety Plan Today
Here’s what to do right now:
- Make a list of every medication, supplement, and OTC drug you take.
- Check the expiration dates on all bottles.
- Move your meds to a cool, dry place-not the bathroom.
- Set up one reminder on your phone for your next dose.
- Write down the three questions to ask your next doctor or pharmacist.
You don’t need to fix everything at once. Start with one step. Then another. Medication safety isn’t about being perfect. It’s about being prepared. And you’re already on the right path by reading this.



michael booth
December 4, 2025Great breakdown. I’ve been managing meds for my dad and this is exactly the kind of clear, no-nonsense advice that saves lives. The six rights thing? I printed it out and taped it to his pill box. Simple, but it works.
Also, the storage tip about not keeping meds in the bathroom? Game changer. Mine were getting soggy from the steam. Moved them to a drawer and now everything’s stable.
Carolyn Ford
December 6, 2025Let’s be real-this is all common sense, isn’t it? Why are we treating this like some revolutionary guide? If you can’t read a label or remember to take your pills, maybe you shouldn’t be managing them at all. I’ve been on 7 medications since I was 28, and I’ve never needed a ‘guide’-just common discipline.
Also, ‘natural’ supplements? Please. If it’s not FDA-approved, it’s a gamble. Stop pretending herbal nonsense is safe.
Heidi Thomas
December 8, 2025You missed the most important point. The real danger isn’t misreading labels or forgetting doses-it’s doctors prescribing drugs without checking interactions. I had a friend die from mixing warfarin with turmeric. The pharmacist knew. The doctor didn’t. Who’s accountable here?
And why are you telling people to use apps? Most seniors can’t navigate their phones. A paper list and a kitchen timer are more effective than any app. Stop overcomplicating it.
Rudy Van den Boogaert
December 9, 2025Just wanted to say this is one of the most useful posts I’ve read all year. I’m a new diabetic and I was terrified of messing up my insulin. The part about storing it properly? I had no idea it could go bad at room temp after a month.
Also, the question about missing a dose-I’ve been doubling up because I thought that’s what you’re supposed to do. Turns out I shouldn’t. Thank you.
Now I’m going to make my list tonight and set alarms. Small steps, right?
Shofner Lehto
December 10, 2025Medication safety isn’t just about compliance-it’s about dignity. People are scared, overwhelmed, and often dismissed by the system. This guide doesn’t just inform, it empowers. The fact that you included the three questions to ask? That’s the kind of thing that gives patients agency.
And yes, generics look different. But they’re not inferior. We need to stop treating them like second-class medicine. Knowledge is the real equalizer here.
Yasmine Hajar
December 12, 2025I’m a nurse and I’ve seen too many ER visits from people who didn’t know what they were taking. This post? It’s everything. The part about not sharing meds? I had a patient once take her husband’s blood pressure pill because he said it helped his headache. He didn’t have high BP. She went into cardiac arrest.
Don’t ever do that. Ever.
Also, if you’re using CBD oil, tell your doctor. It interacts with more meds than you think. I’ve seen it mess with seizure meds, antidepressants, even chemo. Don’t assume it’s ‘just a supplement.’
Karl Barrett
December 13, 2025There’s an epistemological layer here that’s rarely addressed: the patient’s epistemic vulnerability. When you’re handed a prescription, you’re being asked to internalize a complex biomedical protocol without the linguistic or conceptual tools to fully comprehend it.
The Six Rights framework is a phenomenological anchor-it transforms abstract pharmacological data into actionable, embodied practice. It’s not just about adherence; it’s about reasserting autonomy within a system designed to depersonalize care.
And let’s not forget the ontological weight of the pill: it’s not merely a chemical compound-it’s a symbol of trust, authority, and existential risk.
Jake Deeds
December 13, 2025Wow. This is just… touching. I mean, really. How many people are just blindly swallowing pills like candy? I almost cried reading about the bathroom storage thing. My mom used to keep her heart meds next to the toilet. I didn’t even realize it was dangerous until now.
Also, I’m so proud of you for writing this. Not everyone has the courage to speak up when the system fails people. You did. And I’m telling everyone I know. This deserves to go viral.
val kendra
December 14, 2025Love this. One thing I’d add: if you’re on blood thinners, avoid grapefruit. It’s not just a myth. It can make your meds way too strong. My cousin almost bled out because she didn’t know.
Also, if your pharmacy gives you a new bottle and the pill looks weird? Don’t be shy. Walk back and ask. They’ve seen it a hundred times. No judgment.
And yes-use the pill organizer. I use one with alarms built in. Best $15 I ever spent.
Isabelle Bujold
December 15, 2025As someone who’s been managing chronic pain and depression meds for over a decade, I can tell you this guide is spot-on-but it’s only half the battle. The real issue is the stigma. People don’t ask questions because they’re afraid they’ll be seen as ‘difficult’ or ‘neurotic.’
I used to feel guilty for asking, ‘Is this really necessary?’ or ‘Can we try a lower dose?’ until I realized: if I’m the one living with the side effects, I have every right to question it.
Also, Canadian pharmacies often send different generics than U.S. ones. I’ve had to call my doctor twice because the pill shape changed and I panicked. Always verify, even if the name matches.
And for the love of God, keep your meds away from kids. My niece found my anxiety pills once. She was fine, but I had to spend three hours at the ER explaining it. Don’t let that be you.
This guide should be handed out with every first prescription. Period.